
Staci’s Question:
Hello, Dr. D, I was on Biest, 80:20 ratio. One mg/mL. I take one click, which is a quarter gram per day. I have been taking that for two and a half months to come about sleep disturbances, low libido, and hot flushes. I also take 100 mg of progesterone capsules at night. After the two and a half months, my breasts were so dense, tender and sore that I had to stop, to get some of the estrogen out of my body. I still get my period intermittently, so I don’t think I’m quite finished going through menopause yet. Should I lower my Biest dose or take it every other day? The hormones do alleviate my symptoms. It’s just that, eventually, it seems to be too strong.
Short Answer:
For a woman, it is a tough situation to be experiencing hot flashes, but still be mensturating at the same time. When a woman is still mensturating, she is not an ideal canidate for bioidentical estrogen. The fact that a woman is have a cycle means that she is still producing enough of her own estrogen, so taking an exogenous source of estrogen can cause some unwanted side effects like breast tenderness or unwanted bleeding. In Staci’s case, taking progesterone alone might be enough to help aleviate some of her symptoms. Also, supplementing with iodine can help to reduce breast tenderness.
PYHP 082 Full Transcript:
Dr. Maki: Everyone, thank you for joining of another episode of the progressional podcast. I’m Dr. Maki.
Dr. Davidson: And I’m Dr. Davidson.
Dr. Maki: So we’re back at another episode. Again, if you hear weird noise in the background, we have our co-pilot Bob with us. He’s chewing on a beef cheek and he’s making quit of the noise so, let me apologize for that. Like I said, we used to try to redo this with all the background noise but, we just kind of gave up on it because he always has to be right in our feet where we are, and we are to keep from occupied, is to give him something to chew on so. Hopefully, it’s not too distracting but at the same time when we record these, we always listen to the recordings afterwards and you can hear it back there so hopefully it’s not too terrible.
Dr. Davidson: And he likes to push that beef cheek up against the table desk here and it’s got this metal little prod on the bottom that he just likes to push up against it, so that’s why it’s making all that noise.
Dr. Maki: Yes. He’s trying to get some leverage. It’s not as bad as it probably could be, I guess. But it is connected through the table and the microphones are attached to the table and of course, the frame of the table has to be metal. But anyways-
Dr. Davidson: He could be barking.
Dr. Maki: Anyways, hopefully, it’s not too annoying for you. He’ll probably change positions in a little bit and it’ll go away. So, on this one, we’re going to do another question. We have a kind of a backlog of questions, that come in via email and comments through the website. And it is all time consuming, to be able to answer them one on one. That’s why we decided to do these questions on a podcast so everybody get– we have a lot of questions to answer but then everybody gets the benefit from the answer. So, Dr. Davidson, this one is question from Staci so, why don’t you go ahead and read it.
Dr. Davidson: Sure. This is from Staci, “Hello Dr. D. I was on Biest, 80:20 ratio. One mg/mL. I take one click, which is a quarter gram per day. I have been taking that for two and a half months to come about sleep disturbances, low libido, and hot flushes. I also take 100 mg of progesterone capsules at night. After the two and a half months, my breasts were so dense, tender and sore that I had to stop, to get some of the estrogen out of my body. I still get my period intermittently, so I don’t think I’m quite finished going through menopause yet. Should I lower my Bias dose or take it every other day? The hormones do alleviate my symptoms. It’s just that, eventually it seems to be too strong.”
Dr. Maki: We certainly run into these kinds of situations every once in a while. Now, the interesting thing when she says up to the top she says 80. She didn’t tell us how old she is but we’re assuming based on the rest of her question that she’s probably in her like 40s. I would assume probably somewhere between 47, 48, 49 or it say something like that. Would you agree or just say something different?
Dr. Davidson: Yes. I would say definitely late 40s. Maybe 50 but definitely late 40s.
Dr. Maki: Yes. Sure. So she’s on Bias 80-21 mg/g. She only takes 1 click per day. So, when she refers to the word click that’s referring to a device called the Topi-click. Topi-click, the way I kind of describe it, it’s kind of like a deodorant dispenser that has a little dial on the bottom and you turn it, two clicks and a little cream comes up the top, and then you take that cream and then you rub it into your skin. So, she’s only a typical one gram dosage. We’re kind of discussing this ahead of time making sure that, you and I are on the same page. I want you to break that part down which she’s actually taking.
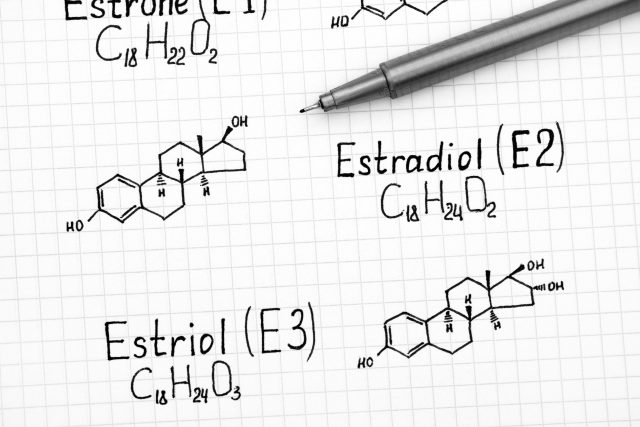
Dr. Davidson: So, yes. She’s taking the cream, the Bias cream. One mg is very actually not that high, but it does have the 80:20 ratio. Meaning, there’s 80% Estriol and 20% Estradiol. So, if she’s only doing one click which would equal a quart of a gram, one-fourth of a gram of cream, that would be 1/4 of 1mg per mL. She’s technically taking 0.25mg which would equal, which isn’t a lot but still, everybody’s different, 0.2mg of the Estriol so E3, 0.2mg of the Estriol and 0.05mg of the Estradiol.
Now, she does say that this is helping her which is great but one thing is, with the bio-identical hormone it’s not [inaudible]. It’s not one size fits all. Everybody is so different. What might work for one person isn’t gonna work for another person and that’s why it’s definitely you’ve got to work with the individual and also work with the doses because she could just be really sensitive to this Biest
Dr. Maki: Yeah right. She also mentioned that she’s still having her cycle intermittently so, in some ways she’s not exactly a hundred percent candidate because she’s still cycling. Now intermittently, we don’t know if that’s every other month, every 3 months which she had 2 periods on the last year, intermittently means that she’s not having one every 30 days. Her body is still producing some of its own estrogen which you put it in your an external source of estrogen. On top of that, which is your may be conservating. but honestly, looking at when I read this the first time, that’s why we’re gonna talk about it because it seemed a little bit odd that she’s having a such an intense respond from taking such a low amount of hormone.
Dr. Davidson: Like I said, everybody is sensitive, everybody is different. She mentions that eventually, this seems too strong which makes sense because she is cycling a bit. So, when you’re in perimenopause, going in to menopause, there’s just phases like puberty. Puberty is several years long. Just like, perimenopause is several years long which be leads in to menopause which menopause is several years long, unfortunately possibly. We want to minimize that.
Then there’s that post-menopause when thee ovaries have for sure definitely retired. Like the ovaries are no longer functioning because she’s having a cycle every once in a while. The ovaries are doing something. They’re not working full time but they’re working part-time or some, so what’s happening is when her ovaries decide to make some estrogen, this extra estrogen she’s taking exogenously is just making it go up a little bit too high.
What I think in Staci’s case because I have so many different patients and some of them are super sensitive and some of them you have to basically give them so much to make any kind of reaction happen, is I think Staci might be one of those super-sensitive individuals to the Estradiol. I think even though it’s such a small, small amount of Estradiol, I think the Estradiol might be having a contributing factor to this.
Dr. Maki: Like what you said too which is a really good point, that eventually if it comes too strong so I guarantee you that as her breast tenderness increases, her cycle is probably right around the corner. So, those are probably coinciding for the most part at the same time. It is like you said her own production is still there, but now you add up just even a little bit and know it’s kind of putting her over the edge. It’s making her really uncomfortable.
Dr. Davidson: When she’s talking about the estrogen, honestly like I said I do think she’s sensitive to the Estradiol and she is having hot flushes so her estrogen level probably is dropping, because like we said she is probably in her late 40s or maybe at 50. Some women are still having a period but she’s probably not beyond 50 years old.
What I would say is the hot flushes more than likely or probably night sweats, because that’s what typically happens when someone’s going from perimenopause into menopause is they don’t necessarily too many hot flushes during the day necessarily. It really is more about having a hot flushes at night. They might be getting hot and tossing the covers around. There he is. He’s making noise.
Dr. Maki: Sorry, he’s growling at his beef cheek down there.
Dr. Davidson: That darn beef cheek huh. But anyways, so she’s probably having more hot flushes at night, maybe even some night sweats so that’s why she’s taking it once per day and definitely I would have Staci take that, as whenever type of estrogen she is going to take, take it at night to help her with sleep because that would help her sleep and that would help with the night time hot flushes.
Dr. Maki: Right. Like you said, the night sweats that covers your coming on and off and on and off so now, she’s waking up probably multiple times. We had women over the years, they tell us they’re waking up 5, 6, 7 times a night. It’s just like every half an hour or every 45 minutes, they’re waking up. They might get that little window of sleep right in the morning usually between like 5 to 7 o’clock in the morning, right? When they’re getting– when they need to get up for the day, they finally get like an hour of decent sleep and then their alarm goes off and they’re literally completely exhausted.
Dr. Davidson: Definitely with the sleeping and I love, hopefully we’re not jumping around here too much for you but I love the progesterone capsules because they do help you sleep. Like she says, I’m taking a 100mg of progesterone at night that does help with sleep so I like that but just on the side note with the breast tenderness and the soreness, is sometimes too much progesterone can actually cause in some individuals that are sensitive, weight gain and water weight gain especially in the breast tissue.
So, it might even be that her progesterone might be just a little bit too high for her, where a 100mg is pretty much like 80 percent that’s like the most common dose when you’re gonna do progesterone as bio-identical hormone replacement is a 100mg. It could be but that’s just a little bit too much for her.
Dr. Maki: What we don’t know it says progesterone is 100mg but there’s also a possibility that could be Prometrium 100mg and that could easily cause breast tenderness. If it is not bio-identical progesterone sustain release, honestly, if that was the case, let’s just say hypothetically because she didn’t specify that the progesterone was actually Prometrium. You get it from a big box pharmacy and she’s taking such a small amount of the Biest, it’s more related to the Prometrium that it would be in the Biest.
Dr. Davidson: Because Prometrium still technically is, it is progesterone. There’s a lot of fillers in it and it seems to be quite a bit stronger than when you have it compounded from your compounding pharmacy. The Prometrium definitely and there’s only two dosings on Prometrium right now. There’s only a 100mg and 200mg. Some people try to break it in half and reduce it but it’s really just better to have it compounded so you have a clean progesterone capsule.
Like Dr. Maki said, you don’t necessarily want instant release because it goes into your system and it goes right out, where the sustained release on the progesterone taking that at night will stay in your system while you’re sleeping. It raises up the gabet[?], lowers the cortisol, it helps you sleep throughout the night and it doesn’t have that effects so much on the water weight, which our breast tissue is very sensitive to water weight.
Dr. Maki: Yeah right. We’d like to think that it is bio-identical progesterone but the fact that she’s just on such a low dose of the Biest, it just makes me think that progesterone which keeps past up Prometrium gets past off as bio-identical progesterone all the time. Because like you said technically it is, but we don’t prescribe Prometrium very often or hardly ever, because most women they just don’t tolerate it very well. This kind of races that red flag that this could be one of those side effects of women seems to experience.
Dr. Davidson: In Staci’s case, I mean let’s say disclaimer disclaimer disclaimer. If somebody came in with this question, what would you first suggest to do?
Dr. Maki: Well, she’s having some definite symptoms, right? She’s having a very classic perimenopausal transition. She can’t sleep, she’s having some night sweats but now, she’s in kind of a tough spot between having a regular period hot flushes but not being able to tolerate the estrogen. That’s a really tough spot to be. Thank God, we don’t really run into that situation very often and it only happens in rare instances that’s not necessarily the most common.
As we are talking about preparing for this episode, I would want to investigate progesterone for sure, maybe lower the progesterone dose, trying on even going down to 25mg, 50mg somewhere in there and then do a simple titration. When you’re taking the Biest with the progesterone, you want to be careful because if you’re taking estrogen by itself, she’s still intermittently menstruating so the progesterone is very important because if she’s just taking the Biest with no progesterone, it’s going to increase bleeding.
It’s gonna make it in very sporadic, it’s just gonna make it more unpredictable because that will create growth to the urinal[?] lining, which is what we don’t want. As a way to establish tolerance to see how she responds at a lower dose, to see if it alleviates and maybe she can acclimate to a higher amount over the period of a couple of weeks.
Dr. Davidson: Yeah probably 75mg I think would be a good dose for Staci, if she’s doing a very low dose of that estrogen, that would probably eventually, she would probably feel a lot better on that. The 25 like you said working our way up would be really great because that way she can see where she feels the best at. I do think that probably ultimately, I would say she would like 75 to 80mg probably would be the ending dose.
Also to with the Biest honestly, her symptoms are the breast tenderness could be coming from the progesterone but a lot of times, it is from estrogen and it’s usually from Estradiol not from Estriol which is E3, it is from Estradiol (E2) which is the strongest. So, I would even consider taking Estradiol right out of the picture.
Dr. Maki: Just to like straight Estriol cream or a straight E3 cream. I mean, she’s not doing hardly any right now, she’s doing literally based on what she wrote here, this is accurate. She’s doing a quarter of a milligram daily. Our usual starting dose for most women is usually 3 to 5mg but like you said earlier, women are sensitive so you have to take that into consideration and every woman’s dose.
Now I will say, where they start and where they end are two different things. Where they start is different and where they end because eventually she’s gonna need more estrogen just guaranteed because more than likely she’s already having symptoms now. Those symptoms are gonna continue as over the next 6 months to 2 years.
Dr. Davidson: We’re not statues. We’re not static. Our bodies are changing from seasons, time, what hormones. Like you said, we always check people’s blood work, we check with them often to make sure that, “Hey it’s time to change a dose, it’s time to re-adjust this.” Taking into consideration the thyroid and the adrenal. So absolutely yeah, this would be kind of a starting would never be her ending because things never end.
I would definitely, honestly, she would probably be a really good candidate like suggesting to her doctor the prescribe Estriol only. I have several, actually a lot. of patients that do really good on just Estriol which is E3 only and I even have them do it twice a day because you gotta love the bio-identical hormones.
They’re amazing, but truly they don’t have a very long half-life. If you’re gonna put on any kind of bio-identical estrogen whether it’s Estradiol or Estriol, you know Biest, let’s say you put it on 8 o’clock in the morning, really by 8 o’clock, 10 o’clock at night, it’s gonna be pretty much out of your system. So, I would do an Estriol, twice a day.
Dr. Maki: Yeah sure, right. And now again, her symptoms. She’s having some sleep issues, got a low libido, she’s got hot flushes. What we don’t know is anything really about her life situation, right? Is her stress level really high? You would see this kind of symptom picture in someone that has a relatively high-stress level.
So supporting the adrenal function, let’s say she can’t even tolerate any Biest. Let’s say we changed it just to Estriol and she still keeps on having the same situation. Supporting adrenal function is another way to you know kind of help, one help improve the sleep and then that might have an impact on the hot flushes as well.
Dr. Davidson: That’s a great suggestion. In fact, I think we should just run on a little tangent on that. So let’s say that Staci is in her late 40s, okay. Unlike us, late gals[?] in her late 40s were kind of stressed out and a lot going on maybe a little overwhelmed. Think about sleep disturbances, low libido, even hot flushes that can all come from the adrenal gland. I even see that women in their 30s.
Dr. Maki: Right. In some ways, the hole mark of going into perimenopause, there’s a drop in progesterone production, which there’s this pathway if you want to call it the Pregnenolone Steal. When there’s a lot of stress going on, your body is very discretionary scars. What things it’s gonna devote energy to. So the Pregnenolone Steal which in functions medicines kind of a common thing but especially when a woman’s going into perimenopause, her progesterone levels are already dropping anyways, but the body will divert all of those basically steroid-based hormones.
Hormones made from cholesterol which all the sex hormones are, including cortisol. Cortisol is a steroid-based hormone. It will divert all attention towards cortisol, so now you have all these cortisol going around because of life circumstances and not sleeping that compounds the issue and there’s no progesterone or female hormones really to buffer that out. That’s the epitome of perimenopausal symptoms. They’re just miserable because they have all these cortisol all the time.
Dr. Davidson: Exactly. Also threw it out there, female libido is really hard. You guys, you guys, you’re a little bit easier on that libido side but as gals we’re so complicated yet we’re so worth it but we’re so complicated when it comes to sex drive and libido. So, when there’s a lot of cortisol going around, there’s not enough sleep going on, you’re tired during the day, the last thing a gal wants to do is even think about sex, let alone engaging that physical activity. It could even be that, that low libido is coming from adrenal glands.
Dr. Maki: Yeah right. Well, if you think about it from a survival perspective not that we have to worry about that in America but maybe with all the Coronavirus stuff, we’re in the kind of survival mode. Everyone on the daily basis going to work and taking care of your family and doing the million things that women have to do on a daily basis, that does put us in kind of a pseudo fight for flight response.
Those stress hormones do arise and when those stress hormones are elevated consistently and lack of sleep, basically constitutes as a separate stress because now your body is not able to recharge itself, the libido is gonna disappear. Your body is worried about surviving, it’s not worrying about thriving or reproducing at that point. The thoughts of the brain, the desire and that’s same thing holds true for men too.
The more stress men have, their libido runs away for the exact to the same reasons. They just don’t have any thought or they are just nothing there whatsoever. In case, like this if you get a sleep under control, you get the hot flushes which affect the sleep, stress is a tough one. How do you tell someone or how do you– There’s no pill you can give to someone or there’s no supplement or prescription to give to someone to help alleviate their stress.
Dr. Davidson: I think it’s called wine.
Dr. Maki: Yeah right.
Dr. Davidson: No, I’m just kidding. That’s a double-edged sword.
Dr. Maki: Right. That has its own issues. That can certainly alleviate or that can exacerbate the odd life.
Dr. Davidson: And the sleep disturbances.
Dr. Maki: Yeah totally. How many people that we know they get home from work, they have a glass or two of wine, it helps them to shake off the day but now their sleep is completely– It’s gonna blow up all night long because they just can’t tolerate that anymore. So, you’re right. It’s a very much a fine line there between wanting to have some wine at the end of the day or a cocktail or a drink or something but you know there’s some consequences.
Dr. Davidson: Or sugar for that matter too because a lot of times when you’re running on high cortisol, you’re not hungry during the day and then you get home and all the sudden at 7:30 at night, it’s like an extracurricular activity to start eating. It’s not carrots and celery, it’s like where are the carbs, where’s the sugar? That will disrupt your sleep.
Dr. Maki: Yeah right. And then, of course, we’re doing that on a regular basis. In a context of a perimenopausal woman, it’s really– a lot of it it’s not her fault necessarily because her body is changing in a way that she’s not really used to, and that’s what we hear from our patients all the time. I mean, I know you’re kind of in the throws of that yourself.
Dr. Davidson: You’re gonna get it.
Dr. Maki: You can really relate and I could really relate too, because you know we’re just teasing. Nonetheless, a woman’s body at this point her life is going through some very drastic changes and we hear it all the time. Women, they don’t know what’s happening. They go to doctor after doctor. The doctors don’t know what’s happening.
I think we’ve done a fairly good job of understanding what’s going on there and more importantly how to help them. In this case, we would possibly switch to progesterone to bio-identical if it’s Prometrium. Lower the dose. We would maybe switch the Biest from Biest to actually just straight Estriol. Maybe keep the same dosage but then allow her to kind of play around a little bit. Like we said, supporting the adrenal function.
Dr. Davidson: Absolutely. Like you said, the adrenals. I do think Staci talking to your doc about possibly switching to that Estriol only because E3 is very gentle. Estradiol is very strong, I mean Estradiol is amazing hormone but it could be a runaway train if you don’t rain in that Estradiol. So, I really think her symptoms might be combined with a little too much progesterone.
She’s still cycling, so she’s still making some hormones on top and maybe but still not a lot of hormones because she’s not cycling every month, it sounds like. But switching to the Estriol, Estriol being so gentle, won’t have the effect on the breast tissue, it won’t have an effect on weight gain and it won’t have an effect– if anything the Estriol will probably help on that mood, help with those hot flushes but not have the negative effects that you see on the Estradiol.
Dr. Maki: Right. Now another little trick, when it comes to breast tenderness that you can use for at any decade or any point in life for women, is using a little bit of iodine. Whatever reason there’s a lot of iodine receptors on the breast tissue using not a mega dose of iodine. There’s a lot of misinformation about iodine. I have a patient right now and I’ve had a quite of few of them over the last years so that are kind of acutely hyperthyroid.
We use mega doses of iodine. We’re talking in the mg amount kind of dosages. In hyperthyroid cases to basically not shut off that, but to kind of calm it down. Most of the time, people don’t need those mega doses if they are deficient, they just need a slight-small amount. In this case, what would be kind of a dose would you recommend for a case like this?
Dr. Davidson: Iodine, in theory, does help with breast tenderness. Fibrocystic density, iodine is awesome for. Like you said, you got to be careful with it because doing too much iodine can actually– If you read all over the internet they say iodine will make your thyroid go high but it really makes it go low. Some cases it will make it go high. Iodine is kind of interesting one. You gotta be careful with it but if somebody’s having really severe fibrocystic density, doing iodine very low dose would be-
Dr. Maki: Yes, the RDA is 150mcg, which is a very minuscule amount. You’re Japanese right? Your mom’s from Okinawa. So every time we go over to your mom’s house, even here at our house, we’re always consuming some type of soup. Every time we go to your mom, she’s putting her wonderfully, delicious, clam soup in my face that has– if you know anything about Japanese cooking, it has kombu dashi.
So, you have some seaweed in there. It’s made with Bonito flakes which is basically fish flakes. In some ways, that bowl of soup is, I wouldn’t say loaded with iodine, but it has a nutritional source of iodine. In that kind of quantity, very small little incremental amount if you’re having and that kind of soup, that soup base with a dashi, the kombu dashi. Kombu is just a type of seaweed, that is going to give you that very low amount on a consistent basis. The body is very good at absorbing nutrients on that fashion.
Dr. Davidson: The sea vegetables are a great way to get a source of iodine and if your body doesn’t want it, it just shuttles it out. As opposed to taking a supplement of iodine. Like I said, I do think it really helps the fibrocystic density for the breast tissue but if you’re gonna take iodine, I do think doing a blood test. I’ve had plenty of patients that had low iodine. We put them on iodine, do a blood test and it’s too high.
Dr. Maki: I would say probably about a thousand micrograms is a starting point some of between 500mcg to a thousand. Then like you say, doing iodine test just to see where it is. It is no surprise, iodine is a deficiency in America or probably around the world except for people that live that consumes sea vegetables on a regular basis. Kombu, seaweed like that is a great source. Nori, the type of seaweed that you wrapped on a sushi roll, that doesn’t necessarily have a great deal of iodine in it.
Dr. Davidon: But it taste so good.
Dr. Maki: It’s good, yeah. Now great, most people are not gonna go out if you’re interested in something like that, doing a kombu dashi. It’s fantastic. Every time your mom makes me some clam soup, I’m never gonna turn it down. It’s so good.
Dr. Davidson: She loves to feed you.
Dr. Maki: Yeah. So, that’s another little trick. Something you can play around with again, just be careful. Don’t get up too high. There’s some products out there on the market that have 6,10,15, 20, 25mg of iodine. We usually like to go, somewhere between 500 to a thousand micrograms of iodine. Let’s say for example, 25mg is 25,000 micrograms. So be careful with that. Lot of supplements have these mega doses.
What you’re referring to earlier, it’s called Chaikoff effect. Iodine, in some instances, can either turn your thyroid on or turn it off. We’ve seen in those high dosage, that it actually tends to kind of reduce thyroid function. That’s why we use it in hyperthyroid cases not necessarily, at least a mega doses in hyperthyroid cases.
Dr. Davidson: And also, Evening Primrose Oil is really gentle. You can use that even for teenagers, evening primrose oil is great for when those hormones are imbalanced to help with breast tenderness. Actually, Evening primrose oil just in general is great for the breast tissue. Whether you have breast tenderness or you don’t, it’s just really nice for breast tissue for that density. Evening primrose oil usually, disclaimer disclaimer disclaimer, but right around a thousand milligram is a really good dose, 500 to thousand really thousand is the best.
If someone has other issues going on in terms of [inaudible] or other issues, fibroids and whatnot, then I usually bumped that evening primrose oil up to two thousand, but a thousand milligrams is really good for the breast tissue. Also, we use a lot is an Indole-3-carbinol and a DIM, that’s another one, that helps bring down the estrogen metabolize.
It doesn’t help bring down your estrogen but everything that gets processed or delivered turns in to metabolize, it needs to be shuttled out. Reducing metabolize can help with that breast tenderness, that breast density. Usually, with DIM like a hundred milligrams in the Indole-3-carbinol (I3C) is usually around 200mg is a kind of a nice dose daily for– if you feel like those estrogen metabolites are a little too high.
Dr. Maki: We covered that pretty well. One last thing I would say about estrogen and like you said about the metabolites is kind of reflect a little bit about liver function. Making sure there’s no major burden on the liver function that includes the wine we’re talking about, alcohol, that includes coffee. If she’s not sleeping at night, she’s gonna be tired during the day so she might be doing more coffee than normal.
Dr. Davidson: High-fructose corn syrup.
Dr. Maki: Certainly High-fructose corn syrup which causes fatty liver disease. All those things the liver cannot be overburden because it cannot process all those things. Then those metabolites start to shift and build up and it can make the situation like these worse. That’s a lot to talk about. This is a little bit of a longer one than we normally do, but this one is kind of complicated.
On the surface it seems simple but when she kind of dive into it, it’s a– how do you help someone like this when they can’t– They’re having hot flushes. Estrogen is Biest is the best place to start. How do you do that when she can’t tolerate it. I think we passed it up pretty well and hopefully if Staci hears this, I’m sure she will or let her know. Hopefully, this will give her some options that she can investigate and hopefully get some relief.
Dr. Davidson: Absolutely. I can go on and on and on with testing, and when to test and how to test but I think this was perfect and definitely shout out to Staci. Thank you so much for your question. In fact, all of you, thank you so much for listening and for reading and for sending in your concerns and questions, we love it.
Dr. Maki: Until next time, I’m Dr. Maki.
Dr. Davidson: I’m Dr Davidson.
Dr. Maki: Take care. Bye bye.
The post What Are The Side Effects of Biest? | PYHP 082 appeared first on .
Discover the common and unfamiliar symptoms that you might be experiencing. Get access to cases of real women with hormonal conditions.

In this episode, we return to a listener’s question regarding thyroid dosing in perimenopause. In our previous episode, we answered Tracy’s question about taking estrogen in perimenopause. Tracy also asked us an additional question about her thyroid doses. Tracy does not have a thyroid gland and has been noticing her dose is continually increasing as […]
In this episode, we discuss a listener’s question regarding perimenopause and estrogen hormone replacement. Tracy is concerned because she is still having a period but also has symptoms of low estrogen. She is not sure if she is a candidate for estrogen therapy since she is still cycling. Tracy’s Question: Hi- you’ve discussed in past […]
In this episode we discuss Jenell’s question she submitted on our website (Ask the Dr). Jennell has been having terrible anxiety since entering menopause and it is really affecting her quality of life. Jenell’s Question: Since starting menopause, I’ve had debilitating anxiety, especially bad in the morning. By evening, It practically goes away. I’m 54 […]
In this episode, we discuss a listener’s question. Amanda is 50 years old and starting to have menopausal hot flashes and weight gain. However, she is most concerned about the heart palpitations she is having. Amanda has had a cardiovascular workout and does not have heart disease. Most people might not be aware, but feeling […]
In this episode, we discuss a listener’s question about perimenopause. ‘Maggie’ is in her 40’s and experiencing severe insomnia with anxiety. She has tried supplements and different doses of progesterone with minimal results. She is having so many ups and downs with her insomnia, anxiety, and hormones. She is wondering how long this is going […]
In this episode, we talk about Mary’s hormone concerns after ovarian failure. She is only 34, and in the last 7 years since her ovarian failure has tried many hormone replacement options, all without the success she was looking for. Let’s Read Mary’s Question: When I was 27 years old I was diagnosed with iatrogenic […]