
Jennifer’s Question:
Hi there! Thank you for this forum! My sister is using the Mirena. I would like to recommend she starts BHRT as she is 49 and has perimenopause symptoms. Is she able to take Prometrium and stay on the Mirena? Thank you in advance
Short Answer:
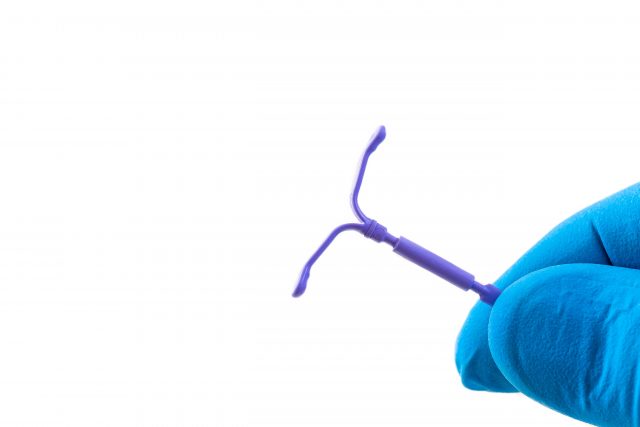
The Mirena IUD contains 52 mg of levonorgestrel, which is a synthetic form of progesterone. This is often recommended for women in their mid to late 40’s to control some of the symptoms of perimenopause. The IUD is fine for pregnancy prevention, but we don’t agree with women in perimenopause given birth control to control their symptoms. There are better BHRT options for managing perimenopause symptoms. However, depending on the woman and her symptoms, she could take progesterone with an IUD. We recommend bioidentical sustained-release progesterone, but not Prometrium. There are more dosing options with bioidentical progesterone and the sustained-release form seems to be better tolerated than the instant-release Prometrium.
PYHP 090 Full Transcript:
Dr. Maki: Hello everyone, thank you for joining us for another episode of the Progress Your Health Podcast. I’m Dr. Maki.
Dr. Davidson: And I’m Dr. Davidson.
Dr. Maki: So good morning. How are you doing today?
Dr. Davidson: I’m doing great. I’m doing fantastic. How are you doing?
Dr. Maki: I’m doing fine.
Dr. Maki: We have a question. This actually comes up quite often talking about different types of contraception. Although this one isn’t exactly about contraception. But we’re going to talk about the Merina. just a little bit. Anyways, why don’t you go ahead? This is from Jennifer which is pertaining to I believe her sister, which is kind of like an indirect sort of thing, but she wants to encourage her sister and to be HRT, but her sister wants to use the Mirena.
Dr. Davidson: Which yeah, it sounds like she is using it. It says, so this is from Jennifer she says “thank you for this forum. Hi there.” You’re very welcome. We love it when we get compliments. So Jennifer says, “my sister is using the Merina, I would like to recommend she starts BHRT, bioidentical hormone replacement therapy as she is 49 years old and has perimenopause symptoms. Is she able to take Prometrium and stay on the Merina? Thank you in advance.” So this is actually a question or somewhat a little bit of a roundabout question that we get all the time because since you know the introduction of the IUD, which is from gazillion years ago with Cleopatra, but now they have hormonal IUDs as opposed to the copper IUDs, and they’ve been around for a long time. But a lot of people ask well, you know my hormones are awry, things are off, I’m in my 40s, I don’t want to take birth control pills when you’re in your 40s is an IUD a good idea and is that going to eliminate all my symptoms, and I’m going to you know feel like I was you know fresh and 18 again.
Dr. Maki: Yeah, I think that is a very common gynecological option, right. Because you know as we’ve talked about before on other episodes they don’t really have lots of options. The fact that she’s 49 on an IUD, I just find that fundamentally just not right. Now from a contraception perspective you and I are not necessarily big fans of birth control. The IUD isn’t really a bad option, even though when it comes to all birth control, none of them are good options. But if you’re trying to prevent pregnancy, you know, the Mirena, some of the IUDs, there’s a few other ones that we came across the Kyleena, the Skyla and the Mirena, they’re all different dosages of the progestin that’s in there.
Dr. Davidson: Yeah, and I have a lot of patients on you know IUD way back when it be, you know, the copper was kind of popular. But I would say if you’re going to do an IUD, I do think the hormonal option is in some ways a little easier to deal with than done some ways. I would say better. The Kyleena and the Skyla, I have a few patients on those they’re you know, they’re fairly new because they have a lower amount of hormones that are secreted from the IUD as opposed to the Mirena. But when you think of, you know women in their 40s like, Dr. Maki said, you know birth control pills my gosh, you know, that’s probably not a really the best option. Especially looking at family and personal history for taking those kinds of hormones, birth control pills, but with an IUD there is, you know hormones that are released from it, but there’s not as much as taking, you know, the hormone systemically or orally and at the same time. You know, we talked about perimenopause all the time, you know, when you hit your mid-40s you know we’re pretty much you know, I’m there too, you know one of the biggest side effects of perimenopause is heavy bleeding, or irregular bleeding, or chronic spotting, and when you look at a female that’s had at maybe a hysterectomy or an ablation where they blunt down or remove the inner lining of the uterine wall to prevent such heavy periods. That’s usually happening to a female in their 40s because of that hormonal change that happens before, you know in perimenopause. So I don’t think you know, I think having the hormonal IUD would thin down the lining of the uterus to help somebody with very heavy periods. But it’s not going to help a lot with the other symptoms of perimenopause that we’ve talked about, you know, sex drive, sometimes the night sweats, you know definitely the irritability, irritability, irritability, irritability.
Dr. Maki: That’s the big one. That’s the one that everyone feels like they’re just frustrated in their fine one minute and they go into a fit of rage the next and they don’t really understand why I like they just can’t tolerate some of the things they used to be able to tolerate. Whether it’s you know family stuff, for work stuff, or all the above their threshold for different stressors has diminished significantly.
Dr. Davidson: And then of course another probably main common symptom in perimenopause is the inability to stay asleep all night. You wake up, either you wake up many times for the night, or you wake up in the middle of the night for you know an hour and a half two hours and you can’t get back to sleep and of course, by the time you are able to get back to sleep it’s time to wake up for the morning. But I do think the, you know, in terms of birth control, you know, in the 40s an IUD is a great option for the birth control in terms of all the different types of birth control out there and if they’re having some irregular periods.
Dr. Maki: Yeah, right. I think there’s a lot better options for a 49-year-old to deal with her symptoms and to put, you know to give her an IUD. And there is a little bit of a limitation when a woman does have an IUD because of that, you know, the progestin part it does you know, I mean, you could obviously give her some bioidentical progesterone on top of that. Maybe it would be a little easier or better if it was one of the lower IUDs, the Kyleena or the Skyla, but if you really had to. Now granted it is inserted, of course, that hormone that is on, that is contained within the IUD is going to degrade over time and that hormone that’s there, you know, this is where the research and development of those types of devices are you know kind of you know paramount that’s where they’re the intellectual property so to speak of that IUD device and that degrading hormone, you know. How long would you say that hormone is viable for when a woman has an IUD inserted?
Dr. Davidson: Each IUD is different, you know, it used to be 5 years now., they have ones that are 10 years, the ones with the lower hormones like the Kyleena and especially the Skyla’s going to run a little bit shorter to have that, you know due to removed and you don’t know how many women I’m sure you too that I talked to him like, oh, yeah, you have your IUD and of course it was time to, you know to switch it out like, you know a year ago, or six months ago, or I need to have you know because best-laid plans even though they last for a long time. We never seem to follow through right away. So but I do like the fact that you can have that in there for a number of years and then have that, you know have it removed or even I have had several women too that had the IUD and they hated it. You know, they just hated it and then you go back in you have a removed. You know hey, it’s a procedure, procedures aren’t fun as we all know, but you know, you can still do it and it’s pretty you know innocuous and you know, not that invasive to have it removed if hate it.
Dr. Maki: Yeah. Sure. Yeah, and I think that we probably end up seeing, now we, I think we have a balance of both. You know, we have a balance of ones that did not respond well and there’s ones that seem to do just fine on it. You know, I still don’t like the fact that it’s promoting an IUD for 49-year-old. I think that there’s a lot better options mainly just some progesterone, right. Just some you know, like the sister, must be doing some of her own. Now that’s always kind of challenging to encourage family members to do certain things. Hey, you should do this, you should do this. That’s in some ways for the sister to figure out on her own but that’s you know that’s between the two of them. But she’s must have had this the one writing the question, Jennifer. She must have had her own positive experience with, about identical hormones. She wants to share that with her sister and I would somewhat agree. I think that there’s a lot of things that can be done better and differently than using the IUD as an option. If you’re looking for birth control. Okay, fine, you know, there’s the lesser of several evils when it comes to birth control. There’s nothing that’s perfect. Everything. Whether it’s an oral birth control pill, or you know, an IUD there’s going to be some issues on some level. I mean, would you agree? Do you have anything else to say about that?
Dr. Davidson: You know, I would say, you know, I have a just like, you know Jennifer asks about her sister if she can take Prometrium and stay on the Mirena, which is fine in some regard. So Prometrium is a, I guess a commercially available prescription for progesterone. It’s instant release, there’s only you know two real doses a hundred milligrams and 200 milligrams. And in one thing that you do find just with women, you know us, women, in our mid-40s, mid to late 40s is our progesterone is low and I have a lot of women that have an IUD and I have them on progesterone because it helps with the sleep, it helps balance out the moods, the moods in the sleep, you know, and it helps a little bit with some of the weight gain and all that jazz that happens with the wonderful things of perimenopause. But I do think, you know, her sister could, Promethium isn’t my first choice because I find a hundred milligrams can sometimes of the instant release can be too strong. It’s too much hormone on top of hormones and people just feel puffy and munchy, and heavy, and kind of like lethargic, we’re doing the sustained-release or even doing a lower. I usually do a lower dose of a bioidentical micronized progesterone. And they seemed, and that seems to balance well. So wouldn’t you agree?
Dr. Maki: Yeah, like you said the Mirena like 52 milligrams of a progestin plus the hundred milligrams Prometrium. That’s a lot. So by using bioidentical progesterone, you can change that dose to whatever you want 50, 75 you know, even 25, if you needed to. You can always titrate, you can always move around you can’t really do that with the commercial types because there’s so few options available. And if they already have the like I say, if they already have the IUD with the hormone there, you’re just trying to compliment that in the gentlest way possible not trying to jam in a bunch more hormone. That you know, she might make her feel worse, you know, on top of that. So and you know, like I say the IUD is going to control some symptoms, some of the bleeding, and the spotting, and some of those things maybe some of the cramping. But it is not going to take care of the other perimenopausal symptoms that are just as prevalent, and that the IUD isn’t really going to have an effect on.
Dr. Davidson: Yeah, but get to answer, you know your question, Jennifer. I would say the Prometrium, you’d want to you know, probably do some testing on your sister being on it, to make sure that progesterone isn’t like through the roof and of course seeing how she’s feeling. I wouldn’t say it wouldn’t be necessarily like I said, you know, I just think it might be a little bit too strong, but for sure when your sister or anybody that IUDs got to come out and maybe you don’t need the IUD for birth control anymore. They always, I always find that we have to do some higher level of progesterone with those women when those IUDs come out because they have this progesterone dive or if they are trying to get their ovaries to kind of re-function, maybe they got their IUD out and you know, they’re thinking about pregnancy. You know, maybe they had an idea in their 30s and they’re thinking about pregnancy and they get that IUD out. They always have a crash in that progesterone. So that’s why definitely doing maybe a higher level of progesterone when she has an IUD out would make her feel so much better.
Dr. Maki: Yeah, right. Yeah kind of after the fact and try to re-encourage and you know when it comes to fertility and pregnancy, progesterone, and even thyroid as well. We never really talked much about thyroid but certainly, progesterone is critically important in that process and you’re right. When using a, for a woman that is younger than 49, by the time a woman is 49 her progesterone production. She’s no longer ovulating which is where the progesterone comes from.
Dr. Davidson: More than likely, but you certainly don’t want to like hang your hat on that.
Dr. Maki: Yeah, she could be one of those rare exceptions, but you know statistically she’s not going to be necessarily ovulating and that’s where the drop in progesterone comes from. And then of course, that’s when all the perimenopausal symptoms show up. So yeah, definitely, you know, I think that you know, the sister is making some, Jennifer’s making some good suggestion for the sister. Whether she’ll listen or not and you and I, just kind of fundamentally like I said have some issues with that because we think there’s a lot better options that can be utilized.
Dr. Davidson: And I like this question and I have a sister and I tell her what to do all the time much to her dismay, but there’s love there, right?
Dr. Maki: Yeah. Yeah. She doesn’t. No, she listens sometimes, she listens, she listens sometimes. Yeah. So, I think that one covers this one, this Merina issue comes up a lot, right? Because this is a very common issue, no, a common concern of women of all the different decades. Because you know, it’s when we say that is being pushed. But you know, like I said from a gynecological perspective, there’s limited options and women are looking for solutions to their issues and they kind of end up coming towards us kind of in the roundabout direction sometimes. But hey, you know what? Like you say we have plenty of women that do just as they do fine, they do better on the marina than they did without it. Then you know, that was the right treatment. But then like you said earlier too, you have had plenty women that just, you know, they can’t stand it and they have to get it taken out early, you know, or they have some kind of complication which to be honest I’d say that doesn’t happen as much as it is much as you think that it would. So, do you have anything else to add about Jennifer or Jennifer’s sister or is this one good.
Dr. Davidson: No, this was great and I’m sure other people have questions about IUDs because this comes up all the time and we’ll probably see because it is a little bit of a trend that you see in and you know with doctors and gynecology is doing IUDs with hormones on top of them. You just have to you know, test for it make sure it’s individualized and that it’s not, you know too much.
Dr. Maki: Right, right, right. And it all comes down about the parties, the individualization is really the key because you could have 10 women that are having similar symptoms, or similar diagnosis, or similar situations. But all 10 of them might have a different, at least from our perspective anyway might have a different treatment, or a different treatment plan. There might be some similarities, or some tendencies that we, you know, lean towards, you know throughout. But there’s going to be subtle differences sometimes significant differences from one case to the next and that’s like I said before too that’s also the good part but also the hard part. You know, how are you able to collectively help everybody you know in a seamless fashion like that. That’s why conventionally you know there’s just limited options and people kind of fall through the cracks of that all the time.
Dr. Davidson: But I do like that she’s you know she’s asking that question for her sister. Which is so sweet but yeah hopefully this makes sense to everyone. And if you have any questions or concerns just reach out and absolutely all you listeners, we appreciate you listening. And everybody that’s reading our blogs and articles, we thank you so much.
Dr. Maki: Until next time, I’m Dr. Maki.
Dr. Davidson: I’m Dr. Davidson,
Dr. Maki: Take care, bye.
The post Can You Take Progesterone With An IUD? | PYHP 090 appeared first on .
Discover the common and unfamiliar symptoms that you might be experiencing. Get access to cases of real women with hormonal conditions.

In this episode, we talk about hormone treatments for perimenopause and menopause. There is a vast distinction between perimenopause and menopause when it comes to treatment options. We often see women who are being treated for menopause when they are genuinely not in menopause. Meet Linda: Linda is a listener who sent us a question […]
Recently, Catherine posted a question on our website about Biest cream, and we knew this could interest our listeners. Biest is a combination of estriol and estradiol, one of the most common forms of estrogen therapy used in bio-identical hormone replacement. There are many doses, ratios, options, and methods of using Biest, so we thought […]
Welcome to the Progress Your Health Podcast! This is a podcast that helps you learn about balancing hormones, especially during perimenopause and menopause. We love hearing from our listeners. If you have a question, please visit our website and click Ask the Doctor a question. Let’s read Brigitte’s question! I have been listening and learning […]
In this episode, we talk about the difference between perimenopause and menopause. Both Dr. Maki and I (Dr. Davidson) have worked with women in perimenopause and menopause since 2004 and sometimes get a bit myopic and technical when it comes to explaining the differences. The other day, a patient of Dr Maki’s asked the question, […]
We recently got a great question from a listener and want to share it with you. This question is about a perimenopausal 51-year-old female. She is still menstruating and having confusion about her hormone testing and the hormone therapy that she is currently taking. She is experiencing some breast tenderness and irritability related to her […]
in this episode, we answered a listener’s question. We love questions from listeners. If you have a question, please visit our website and click Ask the Doctor a question. Here is the listener’s question: I have been perimenopause for at least 4 years now I am 47 and after completing a Dutch test with a […]