Can Vaginal Atrophy Be Reversed?
Quick caveat: This article will dive into some sensitive topics about vaginal atrophy and female sexual health. It will talk about how female sexual activities can be impacted by vaginal atrophy. So it may not be appropriate for all viewers. This is not a crass article but about shedding light on a topic that is not discussed but can very much impact women’s lives. I just wanted to put that out there before you start reading.
What is Vaginal Atrophy?
Vaginal atrophy is also called genitourinary syndrome of menopause (GSM). In your research, you will see these terms used interchangeably. For this article, I will use the term vaginal atrophy for simplicity’s sake.
When the ovaries start to decline in the production of hormones, women can start to notice that they have vaginal dryness. This typically happens in menopause, when the estrogen is not being made. Menopause is a normal, natural part of life. Women can go through natural menopause, which is the cessation of ovarian hormones (estrogen and progesterone), or surgical menopause. Surgical menopause is when a woman has an oophorectomy (removal of the ovaries) which usually occurs with a hysterectomy (removal of the uterus). The removal of the ovaries immediately places a woman in menopause. It is the lack of estrogen that causes the vaginal tissues to atrophy. But what exactly is atrophy?
Because of the lack of estrogen, there will be immature vaginal cells called parabasal cells. Estrogen allows parabasal cells to maturate into mature vaginal cells. Having less mature vaginal cells will cause vaginal dryness, pain with intercourse, and even chaffing of the vaginal tissues with exercise. Vaginal atrophy can make a woman more vulnerable to vaginal infections such as: yeast, bacterial vaginosis, and urinary tract infections. It can even cause the tissues of the vaginal canal and vulva to become smaller. All of these will be explained in this article.
Reading this definition can be helpful but dry (no pun intended). I would like to share some actual accounts to understand how vaginal atrophy can significantly affect women’s quality of life. All identifying information has been removed for privacy. Still, Kathy, Natalie, and Teresa’s stories are real accounts (names and identifying info changed) to help you understand the impact of vaginal dryness. Later in the article, I will go into how to reverse vaginal atrophy using Kathy, Natalie, and Teresa as examples.
The Many Faces of Vaginal Atrophy:
Meet Kathy:
Kathy is a 55-year-old elementary school teacher and single. Kathy had a full hysterectomy (oophorectomy/ovaries and uterus removal) when she was 44 for endometriosis, fibroids, a 6cm ovarian cyst, and heavy bleeding. Trust me, Kathy was so over having to wear nighttime pads during the day. She was tired of trying to get someone to watch her class so she could slip out because she couldn’t go longer than 2 hours between bathroom breaks due to her period. And the pain, chronic spotting, and irregular periods made Kathy more than welcome the total hysterectomy. Kathy’s surgery was a number of years ago, in 2004. This was the time that the Women’s Health Initiative (WHI) study showed that hormone replacement with estrogen and progestin could be dangerous to women’s health.
The WHI study, results, and controversy is a completely different topic. But in short, the study used conventional hormone replacement and synthetic progestins (not bio-identical hormones), the people in the study had other pre-existing conditions and the doses were not proper. The results showed health injury to women taking conventional and synthetic hormone replacement. It ultimately was a positive move forward in ending most of the prescriptions for premarin and prempro, which really can have a damaging impact on a woman’s health. But it put all hormone replacement under scrutiny and even the bio-identical hormones were given a bad rap. But as I said, the WHI study is a whole other topic. Because of the timing and the study, Kathy was not given any hormone replacement after her surgery, so she immediately went into surgical menopause. Instant menopause really was not a problem for Kathy.
She dealt with the night sweats and hot flashes just fine because she was so happy never to have a period again. She was thrilled to be out of pain and didn’t have to deal with those heavy periods that came with the worst unpredictable timing (vacations, at work with 30 unruly 6-year-olds). Fast forward 10 years to 2014, when Kathy came to see me. She said she felt pretty good but had a problem in her ‘female regions.’ A few years prior (she couldn’t remember exactly when it happened), she felt like it was ‘dry down there’ (meaning her vulva/vaginal inner tissues/labia majora and minora). Her vaginal area would feel sore and tender after a long walk or hike from the rubbing. That the vaginal area even seemed smaller and not as plump as it used to be.
She discussed it with her gynecologist when she went in for a check-up. But the gynecologist seemed rushed and said because she had a full hysterectomy, wasn’t sexually active, and was post-menopausal, she didn’t really need pap smears or gyn exams very often. And the doc blew off the vaginal issues that she was asking about. She left feeling dismissed, confused (pap/gyn exam or not, or never?), and still discouraged about the vaginal dryness. There was a catch. Yes, Kathy had not been sexually active since her hysterectomy. But recently, she met someone (Dave) on an online dating site, and they were seeing each other regularly. She was ready to be intimate with Dave but wasn’t sure her body was. She was worried that sex would be painful and uncomfortable (the opposite of what it should be).
Meet Natalie:
When I met Natalie, she was 52 years old. She hadn’t had her period in almost a year and had all the usual menopausal symptoms. She was waking up in the middle of the night sweating so badly that she needed to change her t-shirt. She would get multiple hot flashes throughout the day. She felt tired because of the disrupted sleep and felt like she had a lot of brain fog. She wanted to work on the hot flashes, night sweats, and weight gain. She had gained 20 lbs since starting menopause. Yes, hormones can cause weight gain. I asked her about vaginal dryness and pain with intercourse.
Natalie nodded and said, ‘yes, is that part of menopause? I didn’t know what was happening to me, but it’s very dry down there.’ It was a relief for her to know that it was very common to have vaginal atrophy in menopause. I’m pretty easy to talk to, so Natalie and I had a very in-depth conversation about vaginal atrophy. She admitted that it was affecting her life a lot and would instead work on that before anything else. Of course, with bio-identical hormone treatment, we can work on it all at the same time. Natalie was married with her two kids away at college.
She said being empty nesters was a good time for her and her husband to spend more time together, and they both had very good libidos. It’s just sex was very uncomfortable for Natalie. It made her husband worried and hesitant with sexual relations because he didn’t want to hurt her, and a couple of times, she had some bleeding after sex. That really freaked her husband out when she had bleeding with sex. But that can happen with vaginal atrophy. The tissues can become so fragile that tissues can tear and cause bleeding. Side note: Natalie did have a complete gynecological exam and a pap smear with a transvaginal ultrasound. This was to make sure the bleeding was, in fact, due to vaginal atrophy. If you have having bleeding outside your normal cycle or post menopause (also called abnormal uterine bleeding), have it checked out.
Meet Teresa:
Teresa came to see me for frequent urinary tract infections (UTIs) and vaginal infections. She was at her wit’s end. She had seen a urologist and her gynecologist many times but had no relief. The infections just kept coming back. She had taken multiple rounds of antibiotics for the UTIs. She was told she had yeast infections and bacterial vaginosis (BV). And for that, she had taken multiple antibiotic creams and oral antifungals for vaginal infections. She would take antibiotics and antifungals and get relief for a week to even a couple of months. But the infections always seemed to come back. The vaginal irritation always seemed to be there.
If you have ever had a vaginal infection, like yeast or BV, then you know it can be absolutely annoying. It is like you cannot think about anything else. But you still have to go about your usual day/life and try to act like nothing is happening. BV actually has an odor (no matter how hygienic you are), which can be totally embarrassing. Natalie felt like her vaginal area was on fire, burning and itchy, almost constantly. The UTIs were happening every 3-4 months, which meant more antibiotics every 3-4 months. She was told by her urologist that her urethra (the little tube that goes from your bladder to the outside world) was really short. So the e.coli (the main bacteria that causes UTIs) had a shorter distance to crawl up to cause a urinary infection.
This can be true in many women experiencing frequent UTIs. But all of this didn’t start happening until she was in her 50s. Usually, if the short-urethra theory were the case, you would see that in younger women in their 20s. She did all the post-sex proper hygiene but still kept getting these infections. She thought maybe her boyfriend was giving these infections to her, or they were passing them back and forth. It did seem this all started shortly after they started dating. Of course, they both had full STD/STI testing before they ever got intimate. But still, she was baffled and very frustrated that she kept getting these infections. I assured her that she and her boyfriend (Greg) were not passing anything between them per se. When two people first get together, it is common for women to get an infection (vaginal or urinary or both).
Everyone has their own personal ‘flora and fauna.’ We all have different bacteria, yeast, and microorganisms. Like our gut microbiome, we all have so many different bacteria and microorganisms, and everyone’s is different. It’s like your own personal microbiome/microorganism fingerprint. When two people become intimate sexually, we exchange our personal microbiome/microorganism fingerprints. For women, that means it is common to get a urinary tract infection and/or a vaginal infection. But after a short time, this exchange in our own personal organisms becomes more symbiotic, and no infections should happen. But why did Natalie keep getting all these infections? She read online that she might become antibiotic resistant with all the antibiotic use, which she was terrified of. Natalie was 53 years old and hadn’t had a period in well over a year. In fact, she couldn’t really remember her last period.
She was one of the lucky ones (they are out there) and breezed through menopause. She said she didn’t really have any hot flashes or night sweats. She did mention that she and Greg needed to use a lot of lubricant during intercourse. That even mid-intercourse, they needed to apply more lubrication. She had never heard of vaginal atrophy and thought that was normal because of menopause. Menopause is a very normal natural phase of life. But vaginal atrophy can very much increase vaginal infections and UTIs. The vaginal vault/area has its own pH and microbiome where all the microorganisms are in symbiotic harmony. Vaginal atrophy will alter the pH and the microbiome organisms, making getting infections much easier and more frequent.
Can Vaginal Atrophy be Reversed?
Yes, vaginal atrophy can be reversed. There are many conventional and natural treatments for vaginal atrophy. Let me break down some of the most common treatments, and also I will highlight the ones that work for my patients in my practice as well as what worked for Kathy, Natalie, and Teresa.
Conventional Estrogen Therapy:
I am not a fan of conventional therapies involving estradiol or conjugated estrogens locally. Meaning applied to the vaginal tissues or inside the vaginal vault/canal. These are usually used as creams, vaginal rings, or vaginal inserts. The common conventional estrogen therapy for vaginal atrophy is conjugated estrogens and estradiol. You may have heard of these such as premarin, vagifem, estrace and estring to name a few.
Conjugated estrogens are made from pregnant mares (yes, horses) or can be synthetic estrogens. Estradiol is estrogen that female bodies make but are making less to none in menopause (causing vaginal atrophy). Using synthetic estrogens, conjugated estrogens, or estradiol can have some side effects and risks. Estradiol and conjugated estrogens can cause the lining of the uterus to thicken. We do not want a thickened lining post-menopause.
This can cause spotting, bleeding and can even be a risk for uterine cancer. I know a lot of these estradiol and conjugated estrogens, as local applications, are supposed to be in small doses. But it can still thicken the lining of the uterus. For women that do not have a uterus, I still do not prescribe these medications in my practice. Quite a few women have come to see me on these medications. And when I test their blood work, they have elevated levels of estrogen in their system. That means even though these medications are supposed to be localized to the vaginal vault/tissues, in some cases, it is actually entering the bloodstream.
DHEA (dehydroepiandrosterone):
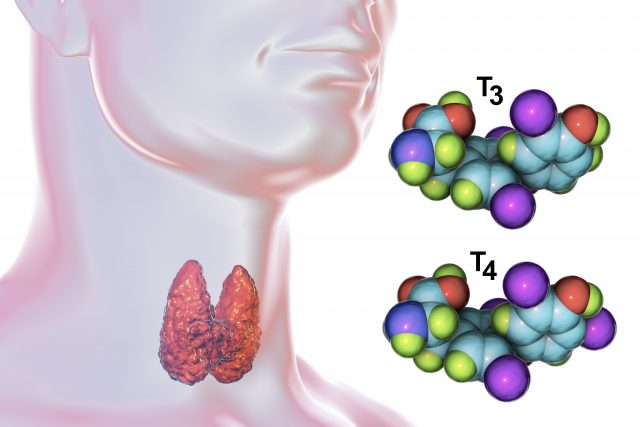
DHEA is a hormone that is mainly made by the adrenal glands. DHEA can convert to testosterone, one of the main ways women have testosterone. The ovaries make a little share of the testosterone. But the conversion of DHEA to testosterone is the primary way that women make testosterone. DHEA topically applied to the vaginal tissues and inside the canal can help vaginal atrophy. Applied locally to the vaginal tissues, the DHEA can convert to testosterone and estroge. The nice thing about DHEA is it will not thicken the uterine lining. The effects are only in the vagina. While DHEA can convert to estrogens and testosterone when applied to the vaginal tissues, it is minimal. So this is not always helpful for all women. Topical DHEA could be very helpful for women with very slight vaginal atrophy. For more advanced vaginal atrophy DHEA may not be strong enough to reverse the atrophy.
There is a conventional prescription for DHEA called Interrosa. It usually comes as a 6.5mg vaginal insert. DHEA can also come from a compounding pharmacy. And there are DHEA vaginal applications available over the counter (in this country, the US). I am not sure about other countries and the availability of DHEA without a prescription. The nice thing about a compounding pharmacy is that you can have any dose or vehicle, such as a cream or suppository. Often the compounding pharmacy will have better pricing than the conventional prescription medication.
Estriol:
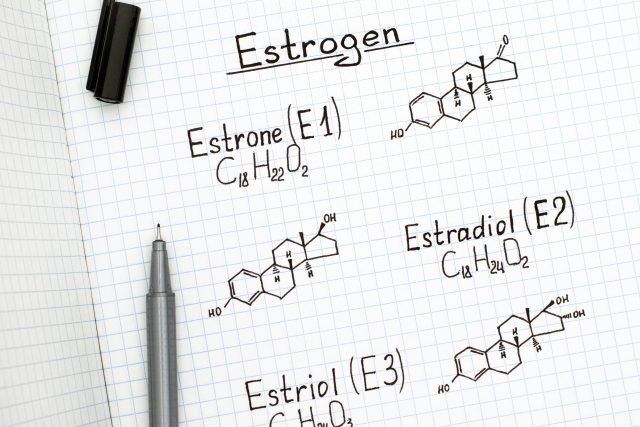
I have found that estriol works very well for vaginal atrophy, and it is safe with less risk than estradiol. Let me explain a little more about estrogens in our bodies. Women make three types of estrogen, estrone (E1), estradiol (E2), and estriol (E3). Most adult women do not make much estrone, which is more common in teens and young women that are just starting their menses. Estradiol is the most potent form of estrogen. It is a great hormone for the heart, brain, and bones, to name a few. But it will cause the uterine lining to grow. That is why women get periods. The estradiol thickens up the lining of the uterus, and if there is no pregnancy, then the lining is shed in a period/menses. Estriol does not have the effect on the endometrium that estradiol does. And using estriol locally will not raise the levels of estrogen in the bloodstream like estradiol can. Remember when I talked about the immature vaginal cells earlier? Estriol can help maturate the vaginal cells. Helping to hydrate and increase the elasticity and resilience of the vaginal tissues. Supplying the vaginal cells with estriol can also help with sensitivity and response to intimate activities. Plus, it is a good choice for women that do not want to take hormones systemically.
Systemic Hormone Replacement:
Systemic hormone replacement is taking hormones transdermally and/or orally. There are many ways to dose hormone replacement. But in short, it is about raising the hormone levels in the blood to target particular symptoms of menopause. There can be many symptoms of menopause. Such as hot flashes, night sweats, brain fog, hair/skin/nails to bone density, and weight management
Using hormone replacement with estrogen and progesterone can also be helpful for vaginal atrophy. I prefer bio-identical hormones because these are hormones that have been made to look exactly like the hormones you would make in your own body. Using systemic hormone replacement can help with other symptoms of menopause while, at the same time, helping reverse or prevent vaginal atrophy. Everyone is different in how they respond to hormone therapy. Although, I have found some women on systemic hormone replacement may need a topical application of estriol for vaginal dryness.
Moisturizers and Lubricants:
Other options for vaginal atrophy are moisturizers and lubricants. Both are different from one another.
Vaginal moisturizers help to enhance the water content in the vaginal cell. While lubricants sit on the surface of the vaginal tissues to help relieve friction with penetration. Lubricants are going to be more effective for vaginal atrophy during intercourse. While moisturizers are used to help the vaginal tissues retain more water/moisture.
Lubricants come as water-soluble or silicone bases. While the silicone base lasts longer (meaning you don’t have to reapply it so often while engaging in sex), it can change the vaginal microbiome. Increasing risk for vaginal infections such as yeast or bacterial vaginosis.
Some women will use natural oils as a lubricant during intercourse. And it can be used as a moisturizer as well to help the hydration of the vaginal cells. Natural oils such as coconut oil, avocado, and olive oil can be helpful for minimal atrophy when used as a vaginal moisturizer. But always do a patch test first to make sure you are not sensitive or allergic.
Moisturizers and lubricants can be helpful in mild vaginal atrophy. Unfortunately, the benefit can be minimal for some women with more advanced atrophy.
Probiotics:
Probiotics with beneficial bacteria can be helpful for maintaining a healthy vaginal microbiome and urogenital health. The vaginal vault/canal and tissues normally have an acidic environment. So the dominant bacteria of the vaginal microflora is Lactobacillus species. Taking a probiotic that contains Lactobacilli reuteri and Lactobacilli rhamnosus can help keep the ecosystem of the vaginal tissues balanced and in symbiotic harmony. This can help prevent vaginal infections and urinary tract infections. Unfortunately, it cannot help to reverse atrophy.
Dilators and Laser therapy:
Using a dilator can help increase the opening of the vaginal canal. I have had women patients come to see me and cannot even have penetration. So it is a process to work with dilators. Make sure to start with a small dilator and slowly increase the width. Some kits have dilators in different sizes, so you can work your way up. Although, this can be very difficult in advanced vaginal atrophy without using some other treatment such as estriol. Just trying to stretch the tissues with a dilator could be painful or result in tearing. Using dilators while doing estriol therapy can have better results than dilators alone.
Laser therapy has become very popular, and it does work for vaginal atrophy. It is non-hormonal, and while helping atrophy, it can also help with urinary incontinence. Although it is an in-office procedure, there is no surgery with vaginal laser therapy. A laser is inserted into the vaginal canal, and the procedure lasts about 5 minutes. You only need a few sessions (around 3), and patients report there is no pain.
What Happened to Kathy, Natalie, and Teresa?
After reading about the treatments for vaginal atrophy, I think it would be helpful to see these treatments utilized in real life. So back to Kathy, Natalie, and Teresa.
Kathy’s Results:
Kathy hadn’t had intercourse for over 10 years since her total hysterectomy. She technically went into ‘surgical menopause’ because her ovaries were removed. But she was thrilled not to have the symptoms she was experiencing before. Fast forward 10 years, and she met a nice man named Dave, and she was really to take their relationship to the next level. But she was terrified that sex would be painful because she did notice that her vaginal tissues were dry and sometimes ached after taking long walks from the rubbing. When I saw Kathy, I explained that this would be a process and that she was a perfect candidate for using estriol vaginally. We used an estriol vaginal insert at night for 5 nights. Thereafter used, the estriol insert twice a week. Again at night because absorption is better and due to gravity, using it during the day can get a little messy. Kathy and Dave had been intimate but without any penetration. After a couple of weeks of using the estriol insert, she noticed that her tissues were more lubricated, plumper, and sensitive to touch (in a good way). I told her that because of this process, they should take their time and aim for penetration about 2-3 months after starting the estriol therapy. And after 2.5 months, they were able to have intercourse with penetration with no difficulty. Now Kathy uses the estriol vaginal insert about once a week to keep the tissues hydrated, resilient, and elastic.
Natalie’s Results:
Natalie had gone through natural menopause and started to notice that sex with her husband was becoming painful and dry. She had a cabinet full of vaginal moisturizers and lubricants that helped minimally. When having intercourse, they had to reapply the lubricant several times because of the dryness. She was also having pretty severe menopausal symptoms, such as terrible night sweats, multiple daytime hot flashes, weight gain, and brain fog. She was even having muscle cramps from all the sweats that were causing dehydration. She was very fatigued because she could not get a good night’s rest from the night sweats. Natalie’s personal health background made her a candidate for systemic bio-identical hormone replacement.
We used a bio-identical hormone cream with a combination of estriol and estradiol (called Biest) and oral bio-identical progesterone. Because Natalie still had her uterus, she needed to take progesterone. I believe when a woman takes any kind of estradiol, she should take progesterone whether she has a uterus or not. But it is especially important if a woman has her uterus to protect her from the risk of uterine cancer. I also had her use an estriol vaginal cream she applied twice weekly for three months. She responded beautifully to the treatment. She was able to sleep through the night, her hot flashes decreased to minimal to none, and she felt a lot more energy and cognitive clarity. Her vaginal dryness and pain with intercourse were alleviated, and now she only uses the estriol vaginal cream once a week or every other week.
Teresa’s Results:
Teresa was at her wit’s end with chronic, frequent vaginal and urinary tract infections. She had been through rounds of antibiotics and antifungals, only to have the infections return. Teresa had been to the gynecologist and the urologist and wasn’t getting any relief. She was starting to avoid sex because the vaginal irritation and burning seemed worst post-sex. And she did all the hygiene and necessary steps post-sex to try and prevent the infections. But they still kept coming back. And she even felt like the vaginal irritation just never left. She had been given an antibiotic to take after intercourse to prevent UTIs. But she didn’t feel comfortable taking medication like that, and even when she did, she still got a UTI.
When Teresa came to see me, she wasn’t feeling hopeful. She said her friend recommended me, and I was her last resort.
All the antibiotics and creams weren’t finding the cause of the infections. So instead of treating the infection, we needed to determine what was causing them. And for Teresa, it all began with her vaginal atrophy. The vaginal vault/canal/area has its own microbiome and pH. Atrophy can disrupt the pH and microorganisms, which can lead to infections. The urethra post-menopause can become a little lax which can cause minor incontinence as well as increased risk for urinary tract infections. The vaginal canal is more acidic. So when the pH rises, becoming more alkaline causes the bacteria species Gardnerella to multiply, causing bacterial vaginosis. To treat Teresa, we needed to change/lower the pH of her vaginal canal and reverse the vaginal atrophy.
Teresa had no other menopausal symptoms, so she did not need systemic hormone replacement. Instead, we did an estriol vaginal insert to help reverse the vaginal atrophy. She used the insert every night for 5nights and, after that, used it three times a week for one month and then twice a week. I also gave Teresa boric acid vaginal capsules to insert post-intercourse. Boric acid vaginally is an old-school treatment for the urogenital system. Boric acid is not painful to the vaginal tissues. It lowers the pH of the vaginal area to help prevent chronic bacterial vaginosis and urinary tract infections. I also had Teresa take a good female probiotic with the main beneficial bacteria that colonizes the vaginal canal. I gave her Women’s Ortho Biotic by Ortho Molecular Products to take daily. It contains the main species in the vaginal vault, Lactobacilli reuteri, and Lactobacilli rhamnosus.
Resource Glossary: Where do I get the treatments/therapies/remedies this article discusses?
I know this was a lengthy article, and I hope it helped you understand vaginal atrophy. How vaginal atrophy can present in many forms and the impact it can have (Kathy, Natalie, and Teresa). As well as the various ways to reverse it. Some of the treatments mentioned in this article are by prescription only. But there are products you can buy without a prescription. Below I provided you a list of some of the products you can buy without a prescription. While I do not work for these companies, I do sell them on my website. So the links that are provided will send you to my website—I just wanted to put that out there for full disclosure.
Estriol:
Estriol can be bought without a prescription (in this country, the US). Below are estriol vaginal inserts:
Hydration ovals by Bezwecken
1X Plus: contains Estriol and DHEA 1mg
2x Plus: contains Estriol and DHEA 2mg
DHEA:
DHEA can be bought without a prescription (in this country the, US). below are DHEA vaginal inserts/suppositories by Bezwecken:
DHEA ovals 13mg
Rewned Vaginal Suppositories 6.5mg
Correcting the pH of the Vaginal Canal/Vault/Tissues:
Yeast Arrest by Vitanica:
This has boric acid plus other healthy ingredients for the vaginal flora. I use this to help correct the vaginal pH.
Probiotic:
Ortho Biotic Women’s by Ortho Molecular Products:
This is the probiotic that has the main species of beneficial bacteria in the vaginal vault/area. Those species are, Lactobacilli reuteri and Lactobacilli rhamnosus. It helps keep the pH in line and balance good and bad bacteria, which can help prevent vaginal infections.
Have questions about your hormones or vaginal atrophy? All questions are welcome and encouraged. Just click on the link, Ask the Doctor.
Thank you for reading,
Dr. Valorie Davidson, Dr. Robert Maki &
Progress Your Health Team
All content found in this blog, including: text, images, audio, video or other formats were created for informational purposes only. The purpose of this website and blog is to promote consumer/public understanding and general knowledge of various health topics. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Please consult your healthcare provider with any questions or concerns you may have regarding your condition and before undertaking a new health care regimen. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. If your healthcare provider is not interested in discussing your health concern regarding this topic then it is time to find a new doctor.