Do I Have Polycystic Ovary Syndrome?
What is Polycystic Ovary Syndrome?
Polycystic Ovary Syndrome or PCOS is merely a condition in which the ovaries present with many cysts. The word poly means many. On ultrasound, the ovary may look like a sac containing a string of pearls or a row of marbles. These so-called pearls or marbles are the cysts which are eggs that were never released from the ovary. They were not released in the monthly menstrual cycles, instead retained in the ovary.
When an egg is released from a follicle in an ovary, we call it ovulation. When the egg is not released during the monthly cycle, then it is referred to as an anovulatory cycle. The most common cause of an anovulatory cycle is PCOS which is a result of hormone imbalance. According to the PCOS Foundation, it is one of the most common hormonal disorders in women. PCOS was initially named the Stein-Leventhal Syndrome because of the two gynecologists, Stein and Leventhal, who discovered it in the 1920s.
When they surgically explored the ovaries of women who were obese, infertile and experiencing menstrual irregularity, they found that the ovaries were enlarged two to four times their normal size and full of tiny fluid-filled cysts. Stein and Leventhal biopsied the ovaries by taking out wedges of the ovary. Much to their surprise, they discovered that the women began regularly menstruating after three to five months and many were able to conceive, all due to the surgical reduction of the enlarged ovary.
The reason for this is not entirely understood. Perhaps it is because after the wedge resection there was a rapid reduction in all ovarian hormones which restored feedback to the hypothalamus and pituitary, resulting in balance once again.
How is PCOS Diagnosed?
PCOS is an endocrine disorder creating a hormonal imbalance that affects women early in their reproductive age and even beyond the reproductive years. There is not a well-defined PCOS test that will give a definitive diagnosis. It was not until the early 1990s, the National Institute of Health sponsored a conference on PCOS. It was here that a formal diagnostic criteria was proposed and utilized. If either androgen or ovulatory issues were present, then a diagnosis of PCOS was given. (More information on androgen and ovulatory problems are discussed in the next section on symptoms)
In 2003 a group of experts in Rotterdam established the criteria still used today. It incorporated the size and morphology of the ovaries determined by ultrasound as part of the criteria. A PCOS diagnosis can be given if a person presents with 2 out of 3 of the criteria:
- Androgen issues
- Ovulatory issues
- Polycystic Ovarian Morphology
What Blood Tests for Polycystic Ovaries?
Comprehensive testing and clinical history are so important so that your doctor can tell what is causing your PCOS symptoms. Insulin can be the problem, but it may not be an insulin-based PCOS. It may be an adrenal problem.
Some important tests for PCOS to run that would be ideal are listed below: (fasting)
- Complete Blood Count
- Comprehensive Metabolic Panel (CMP)
- Lipid panel (triglycerides)
- Liver enzymes – AST / ALT (part of CMP)
- Glucose, fasting (part of CMP)
- Insulin, fasting
- Hemoglobin A1C
- Highly Sensitive C-Reactive Protein (CRP-hs)
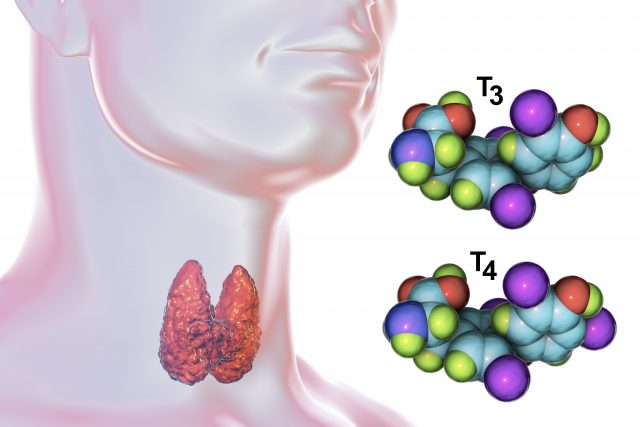
- Thyroid Stimulating Hormone (TSH)
- Free T3
- Free T4
- FSH / LH
- Testosterone, total
- DHEA-S
In some situations, it may also be helpful to run a dried urine test (DUTCH) for hormones as well. This will give us a good picture of what your adrenal glands are doing and if your PCOS symptoms are adrenal based. We can look at the androgen hormones as well as estrogen and progesterone, the female hormones.
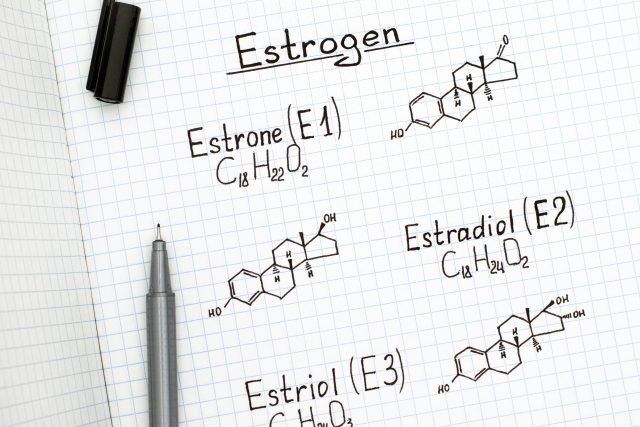
Estrogen is metabolized in the body through different pathways. Some are more potent than others, and it is important to metabolize down a pathway that is less estrogenic with less risk of cancer, and also for estrogen to be in balance with progesterone. Testosterone is also metabolized down different pathways, and we can tell if you are metabolizing through a more potent androgenic pathway which would play a significant role in PCOS symptoms. We just recently had a patient who did this test, and we were able to advise a lifestyle change with targeted supplements since she was experiencing PCOS.
The test revealed that she had high testosterone, high estrogen with lower progesterone and she was sluggish in her clearance of estrogen in the liver. She had symptoms of acne, excess facial hair and heavy irregular periods. Within a month of our protocol, she was all smiles and her complexion cleared and her period was normal. This has been a few months now and her periods are still normal after many years of not being normal.
What are the Symptoms of PCOS?
Androgen issues: Androgens are technically male sex hormones. But women also naturally produce androgens at lower levels. It is when these androgens are excessive that problems arise. DHEA and testosterone are the primary androgen hormone. When a woman produces too much DHEA or testosterone, she can experience androgen issues which are listed below.
- Male pattern baldness
- Thinning hair
- Acne
- Deep hoarse voice
- Anger
- Irritable
- Mood swings
- Skipping periods
- No period at all (no ovulation)
- Hirsutism
- Weight gain
- High blood pressure
- High cholesterol
- Pre-diabetes
Note: Hirsutism is the presence of thick, long, and dark hairs in females in a male-like distribution such as excess hair on the face, chest, inside the thighs, and the belly. These are signs of PCOS in women who also have higher than normal levels of testosterone or DHEA.
Ovulation issues: Have you tried unsuccessfully month after month to become pregnant? This can be so disappointing. If so, you are not alone. Many couples struggle to conceive, only to find out that PCOS is the culprit. PCOS is the leading cause of infertility.
Ovulatory issues include irregular cycles (missed, heavy, or prolonged cycles) which in turn causes infertility challenges.
What Does a Normal Menstrual Cycle Look Like?
Unfortunately, many women with PCOS do not know a regular menstrual cycle because they rarely have one. By understanding the normal cycle, an irregular cycle is better understood. Day one is the first day of your period. Count the days until the first day of your next period. A normal cycle will last from 25-35 days from the start of your period until the start of the next.
The ovary will release an egg mid-way through the cycle for fertilization. If the egg does not become fertile, the shedding of the uterine lining begins. This is the visible blood and the first day of the period. The blood should be bright red in appearance, instead of dark red or brown, and with no clots. These cycles should be consistent month after month. Many women experience PMS, but this is not the norm. It is an indication of hormonal imbalance. It is a good idea to keep a history of your periods so that you can tell if they become irregular and not normal for you and so that you can share your record with your doctor.
How Does Polycystic Ovary Syndrome Cause Infertility?
The effects of PCOS on the ovaries can hinder the production and release of eggs. Thus, ovulation (release of an egg) does not occur. When an egg is not produced and released from the ovary, then an anovulatory cycle occurs. Bleeding still occurs with an anovulatory cycle, but there may be a heavier than normal flow. This is due to the hormonal imbalance caused by the anovulatory cycle. Unreleased eggs stay in the ovary and become the cysts in the polycystic ovary syndrome.
What is the Main Cause of Polycystic Ovary Syndrome?
The function of the ovary is to produce eggs and release hormones which result in the menstruation cycle. Of course, if this doesn’t happen as it should, the ability to conceive is quite impossible. PCOS is to blame in many cases but how does one get PCOS? While researchers can’t agree on the exact cause, many believe that the body’s production of too much insulin may be the root of the issue.
Insulin is a hormone produced by the pancreas in response to food intake, especially carbohydrates. Insulin is responsible for escorting glucose (sugar from the carbs) into the cells where it needs to be. Over time, due to poor diet and lifestyle choices, more and more insulin is required in order to keep blood sugar in check. Eventually, the cells become less sensitive to insulin’s knock at the door to let glucose in, and they become insulin resistant. This causes even more insulin to be produced. If the pancreas senses that sugar is still high in the blood it will continue to produce more insulin to try and move the sugar from the blood into the cells. Thus high insulin is prevalent.
Excess insulin, in turn, can make the ovaries produce too much testosterone (the dominant androgen sex hormone in men). This excess testosterone creates a hormonal imbalance and prevents the primary female hormones, estrogen, and progesterone, from doing their job. Estrogen and progesterone are responsible for producing and releasing an egg for fertilization. If the eggs do not get released from the ovary, then these fluid-filled egg cysts remain in the ovaries.
In some cases, there are women who experience PCOS symptoms, but they are not insulin resistant. There are some women that do not have cysts on their ovaries nor are they overweight. They do not seem to fit the bill for PCOS. Remember that insulin drives up testosterone? So what would drive up their testosterone in these cases? We would look to another gland for the answer – the adrenals. The adrenals and the ovaries both produce 25% testosterone and 50% androstenedione. Androstenedione is a precursor to testosterone. DHEA and DHEA-S are also precursors to testosterone. The Ovaries produce 20% of the DHEA, and the adrenals produce 80% of the DHEA and 100% of the DHEA-S. So a woman could have PCOS symptoms out of either her imbalance in the ovaries due to insulin resistance or in her adrenals with a hypothalamus – pituitary – adrenal dysfunction. It is also possible that a woman can have an issue with both glands at the same time.
|
Androgens |
Ovaries | Adrenals |
Fat Tissue |
| Testosterone |
25% |
25% |
50% |
| Androstenedione (precursor to testosterone |
50% |
50% | |
| DHEA (precursor testosterone) |
20% |
80% |
|
| DHEA-S (precursor to testosterone) |
100% |
Genetics can also play a role in PCOS. We are making great strides in genetics, but we are still just on the horizon with the majority of knowledge in this area yet to be discovered.
Is there a Treatment for PCOS?
Once you know what PCOS is and you understand that you have this issue, you may ask “What can I do about it?” What is the cure or treatment for PCOS? Most people will do an internet search for the answer and find these disappointing words – “There is no treatment yet.” It is true. There is no single medication that will deliver a quick fix. Conventional treatment is often focused on individual symptoms and not the underlying cause. Some medications that are commonly prescribed for PCOS are Metformin and Spironolactone.
While there is no quick fix to PCOS, there is some good news! Simple diet and lifestyle modifications show favorable effects.
What are the diet basics for someone who has PCOS? Most women have high insulin and androgen levels with PCOS. High insulin causes a spike in androgens. So a diet focusing on reducing insulin would be particularly beneficial for an insulin-based PCOS. Insulin goes up after you eat or drink, especially if you consume carbohydrates.
What Not to Eat With PCOS?
- sugary drinks, sodas, juices, alcohol
- grains such as crackers, bread, cookies, pasta, rice, cereal
- candy, chips, and processed snacks.
Some Diet Tips to Consider for PCOS:
Not all carbohydrates are the same. Not all are bad for you. Vegetables and fruits fall into the carbohydrate category too, but they are not the same. They contain many vitamins, minerals, phytonutrients, and fiber. These nutrient-rich carbohydrates are a much better choice.
Imagine a plate loaded with pasta (refined carbs). Imagine also another plate loaded with broccoli (fiber-rich carbs). They are both considered carbohydrates. Which dish do you think will cause the greater insulin spike? Pasta, correct! Refined carbohydrates are quickly digested by the body. This causes a sudden sharp rise in insulin. Fiber-rich carbohydrates are slowly digested. This keeps you from a sudden high insulin spike.
As you can see, the types of carbs in your diet play a significant impact on how your body responds. Not only does the plate of broccoli contain fiber-rich carbs, but it is also considered low carb. Fiber-rich low carbs are very nutritious and help to keep you from insulin spikes.
- Cut out sweet drinks: Save your carbs for food. Don’t waste them on drinks. A pint of orange juice can go down fast without much thought about carb content. With none of the fiber and only pure juice, it gets absorbed rapidly. A good alternative to fruit juice and sodas can be sparkling water. The home soda machines are fun. Add the following to a pint of chilled carbonated water: 5 drops of liquid Stevia, a couple of drops of orange essential oil, and one teaspoon of raw apple cider vinegar. Consider also the many herbal teas on the market.
- Limit bread consumption: Consider purchasing the thinly sliced bread from the market. Two slices make up one slice in thicker cut bread. Look for low carb bread recipes on the web. There are many. For sandwiches use large lettuce leaves as an alternative to bread. Roll up your sandwich filling in lettuce leaves. If you do consume grains, it is best to consume organic grains. Glyphosate, which is a chemical in Round-Up, sprayed on the plants can block an enzyme in the body. This enzyme is important for converting testosterone into estrogen. Remember, most PCOS patients have high testosterone.
- Choose PCOS friendly snacks: Good choices are nuts, seeds, cheese, fresh cut vegetables (carrot/celery sticks), avocado, pepperoni slices, eggs, olives, pork rinds, beef jerky, or hummus.
- Choose high fiber lower carb fruits. Granny Smith apples, plums, blueberries, raspberries, blackberries, and strawberries are good choices. Limit the highest carb fruits like bananas, pineapple, pear, watermelon, grapes, and mango. You would also want to avoid dried fruits since they are dehydrated and the sugar content is concentrated.
- Eat a low carb breakfast: Most people experience a higher insulin spike early in the morning. Choosing a low carb breakfast would be wise. Consider eating leftovers for breakfast like baked chicken or chicken salad. Other considerations include salmon, eggs, omelets, avocados, lunch meats, bacon, and sausage. Try a high-quality protein powder with coconut milk and the lowest carb fruits mentioned above. Throw a few spinach leaves in for good measure.
- Use sugar substitutes: Monk Fruit, Stevia, Xylitol, and Erythritol are excellent choices.
- Choose low carb dairy: unsweetened yogurt, cottage cheese, sour cream, butter, and kefir. Alternatives to dairy include unsweetened nut milks such as almond, coconut, hemp, hazelnut, macadamia, and cashew.
- Track your carbs: If you remove the unhealthiest carb sources from your diet, you’ll be well on your way to improved health. Many people want to go a step further and know how many grams of carbs they may consume in a day. This number can be different for each person who has PCOS. But generally, for PCOS, your number should fall somewhere between 20-150 grams daily. My Fitness Pal online is a great place to keep track of what you are consuming daily. It will help you decide how many calories and macronutrients, such as carbs, are right for you.
- Consume 30 grams of flaxseed daily: Flaxseeds are very fiber rich. 30 grams is about three tablespoons of unground flaxseed. Buy a coffee grinder. Grind a week’s worth and store in the refrigerator. Sprinkle on salads, in yogurt, add to smoothies, or add to mayonnaise. I like it sprinkled in a little bit of unsweetened applesauce for a nutty treat. There is a study done on the effects of flaxseed on hormonal levels associated with PCOS. The patient in this study consumed 30 grams daily for four months. After four months, there was significant testosterone (free and total) reduction. (Pub Med study – PMCID: PMC2752973)
Many women have PCOS, and they don’t even know it. It goes undiagnosed because there is usually a combination of signs and symptoms and many doctors will not dig deep enough to find the root cause. They instead will treat the symptom with yet another drug. Usually, it is not just one thing or one test that will be definitive. I hope this post has helped you become aware of your options and choices. May you find great success in your health by implementing some of these strategies. If you have any questions about PCOS and your diet, please contact us. We offer treatment, testing and specific supplement recommendations for people with PCOS all over the world, and we will listen to your story so that we can get to the root of the problem.
Hopefully, this article gave you some more awareness regarding PCOS. If you have any questions feel free to leave a comment below or send an email to [email protected].