What Bioidentical Hormones Should I Take?
Bioidentical Hormone Replacement Therapy (BHRT) is what I have specifically been working with for the last 14 years. I am not your primary care physician and not your general practitioner. I am a hormone doctor and only work with patients that need hormone balancing. I have treated patients from 14 years old to 70 plus years old for hormone balancing. I do not claim to know everything about hormones. As every doctor has their way of treating hormone imbalance and dosing hormones.
I am going to write this blog from my own personal experience of working with patients and BHRT for the last 14 years (2004-2018 and going). To understand which BHRT may work for you, I want to break down some important aspects of BHRT. There are many conditions that BHRT can help. For this post I am will be focusing on PMS, Menopause, and Low Testosterone. I will go into Thyroid and Adrenal BHRT in another post.
What is BHRT?
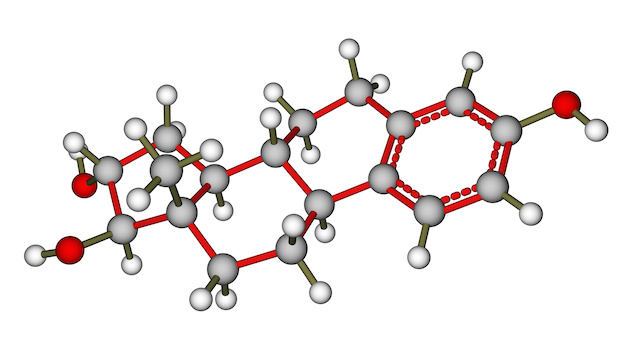
BHRT stands for Bioidentical Hormone Replacement. It is used to replace or help restore hormones in the body that are not being adequately made. Bioidentical means that the hormones you take are exactly identical to the hormones that are made in your body. BHRT is often confused with HRT. HRT stands for hormone replacement therapy. HRT encompasses all hormone replacement, bioidentical or synthetic. Meaning HRT may not involve bioidentical hormones. For example, taking Premarin for menopause used to be commonly prescribed. But Premarin is not a bioidentical hormone because it is actually hormones from horses (pregnant horse mare’s urine to be exact).
So if you are on HRT, make sure to find out that it actually is bioidentical BHRT. If the hormones look exactly like the hormones that we make in our bodies, means it will work exactly as it was intended in the body. This can reduce the side effects and risk factors. I have been treating patients with HRT since 2004, and I have seen they have a much better response to BHRT than non-bio-identical HRT.
What is BHRT used for?
BHRT can be used to correct hormone imbalance or replace hormones that are not being made by the body. Here are the most common examples of what BHRT is used for.
- PMS
- PCOS
- Perimenopause
- Menopause
- Hypothyroid
- Adrenal Fatigue
- Low Testosterone also abbreviated ‘Low T.’
To keep this post from being incredibly long, I am going to focus on menopause, PMS, and low testosterone. I will leave the adrenals and hypothyroid for another blog.
First I want to explain a little more about BHRT. Where to get it, what formulations and dosage it comes in. I will then elaborate on my experience prescribing BHRT to help these conditions (menopause, PMS, and Low T).
Where to get BHRT?
Any doctor with prescriptive rights can prescribe BHRT. To prescribe testosterone, the doctor needs a DEA#, as that is a controlled substance. If you are interested in BHRT, make sure the doctor you see has prescriptive rights to prescribe those particular hormones. Not all doctors specialize in hormones or know what dose is right for the patient. Some doctors refuse to prescribe BHRT. Rightly so, if their experience is limited.
Most often you will find functional medicine doctors and gynecologists prescribing BHRT. But any doctor with an ND, MD or DO after their name can prescribe BHRT. Prescribing BHRT is really an art. There is no “cookie cutter” dose for all patients. Everyone is different as to what their BHRT goals are. Personal and family history differs in all patients, making dosing and prescribing BHRT unique for each person.
Also how a person responds to the BHRT, the doctor or doctor’s assistant needs to be accessible. As there could be a reaction or a quick dose change needed. A patient having a reaction to a particular dose of BHRT should not have to wait 3-5 weeks to get in to see the doctor about it. Every doctor needs to start somewhere when treating patients with BHRT.
Unfortunately, BHRT is not taught in medical school or university to any real depth. Sure, seeing a highly experienced doc with long years in practice and thousands of patients is indeed a good idea. But do not be afraid of the new practitioner dealing with BHRT. They are going to be eager, easily accessible, and not only up on the latest research and continuing education courses, and they won’t be tired and burnt out.
If your primary care, general practitioner, gynecologist does not routinely prescribe BHRT, do not listen to their opinion. If they do not have experience, have not done the continuing education courses, or researched BHRT (Google does not count), then they are not a useful resource as to if BHRT is right for you. I will go on to elaborate on where you get BHRT prescription below. As BHRT can be available from your big box pharmacy. More commonly BHRT is available from a compounding pharmacy.
What Is a Compounding Pharmacy?
A compounding pharmacy is the most common place you can get bioidentical hormones. A compounding pharmacy can make any dose of any hormone you would like. Conventional pharmacies usually only have set doses and preparations of prescriptions. But with a compounding pharmacy, they can make any dose or formulation necessary for the patient.
What forms of BHRT are there?
Formulations should be customized to the patient. But for the most part, BHRT can come in any form you can imagine. The most common types of BHRT are capsules, cream, patches, troches, tablets, gels, suppositories.
BHRT also comes in pellets that are surgically implanted into the gluteus area of the body. Pellets are a minor surgery that is done in the doctor’s office. Pellets are an entirely different blog on what and how that is given/dosed.
The formulations of BHRT are dependant on the particular patient and their personal and family history.
Capsules: Estrogen capsules are not common. Estrogen taken orally is not easily absorbed and puts a burden on the liver. If a person is taking estrogen orally, their liver enzymes should be regularly monitored. Quick side note, estradiol tablets are prescribed. It is not a common practice now, but you will find some docs that do this. But again, it is hard on the liver, and you do not want to take high doses of estradiol.
-Progesterone is often given as a capsule or orally dosed. If a female has a uterus and is taking any kind of estrogen therapy, she must take progesterone. Estrogen will thicken the uterus without progesterone. Progesterone will keep the lining of the uterus thin, so there is no bleeding or a period. It is important to note that taking estrogen without progesterone in a woman that has a uterus, is a risk factor for uterine cancer. If a woman is on estrogen therapy and has a uterus, progesterone is given orally. As progesterone in a cream form is not as effective at keeping the lining of the uterus thin enough.
-Testosterone is rarely, never given as an oral prescription. Testosterone orally is not easily absorbed and puts a burden on the liver. Over time taking testosterone orally can cause liver inflammation.
Creams and Gels: Estrogen (estradiol and estriol) are commonly given as a cream. Testosterone is usually always given as a topical cream. Progesterone is common as a cream. There are gels available. But creams seem to be used more often over gels. Creams and gels are applied to the skin and absorbed transdermally. Some creams are made especially for the vaginal tissues and use transvaginally. Cream and gels not intended for the vaginal tissues should be applied to the inner thigh. If you apply your hormone cream/gel to your inner arms, then it can be shared with other people and animals. This is why I do not advocate applying hormones to your arm. I have seen it get on children and pet too often. The inner thigh is a good place to ensure the hormones will not inadvertently get on others.
Injections: Some doctors do estrogen injections, but that is not common. Testosterone can be given as an injection. Although, it is easier to monitor the dose when the testosterone is a cream. Some men cannot absorb a cream and need an injection of testosterone. Injections can be given in office, or some patients will pick up the injection prescriptions and inject themselves.
Patches: Patches are commonly prescribed for estrogen replacement. There are only a few fixed doses: 0.025, 0.0375, 0.05, .075 and .1mg of estradiol only patches. Patches are applied twice a week.
Troches: Troches are commonly used as sublingual administration of BHRT. Hormones in a troche are absorbed readily. But some patients complain about the taste and the length of time the troche takes to dissolve.
Tablets: Tablets are more common for conventional preparations of estradiol. They are usually given once a day in the morning. Again oral forms of estrogen can place a burden on the liver and are not as commonly prescribed as much currently.
Suppository: Vaginal suppositories are used most commonly for vaginal atrophy. Usually, an estradiol and estriol combination or estriol only is used. Some doctors use vaginal capsules instead of a suppository as it is less messy. But vaginal capsules are less readily absorbed than suppositories.
Vaginal Rings: Vaginal estradiol rings are used for BHRT. They are not that common as they are fairly strong forms of estradiol. Estradiol vaginal rings that are inserted for three months at a time.
Rhythmic Dosing: Rhythmic dosing of estradiol and progesterone is great for menopause. It actually is dosed following a female’s natural 28-day cycle. I think this is a great way to provide BHRT and I will discuss in a separate blog post.
What Types of BHRT are there?
In this section, I want to talk about the types of BHRT. This may overlap a bit with the above formulations. But in this section, I will go more into depth about how the different hormones are prescribed.
-Estradiol: Estradiol is the most common hormone used in menopause. It comes in many different forms and doses. Estradiol formulations and dosages are dependant on the patient’s health history, family history, and BHRT goals.
Conventional preparation: Estradiol is prescribed and can be found at your local big box pharmacy. Estradiol from your traditional big box pharmacy is commonly in the form of tablets, gels, and patches. More rarely, estradiol can come in the form of an estradiol ring vaginal insert. There are also vaginal topicals of estradiol for vaginal atrophy.
Compounded Estradiol: These are formulations that are made from a compounding pharmacy. Estradiol from a compounding pharmacy can come in any dose necessary for the patient. Commonly estradiol is combined with estriol in the form of biest which I will touch on in a bit.
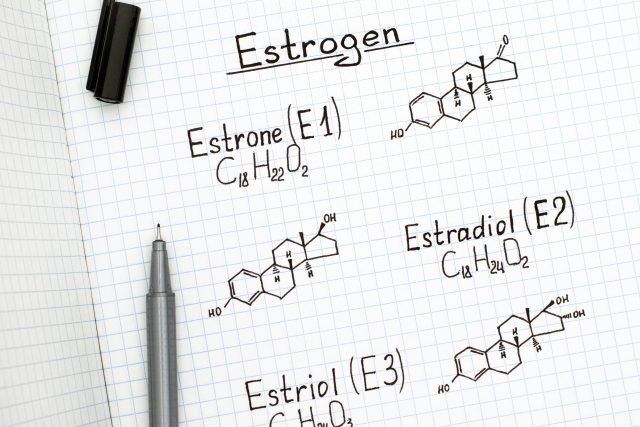
-Estriol: Estriol is the gentlest form of all the bioidentical estrogens (estrone and estradiol being the others). It is often used for vaginal atrophy and vaginal dryness. Estriol is also used to for the facial skin to help with wrinkles. It can come as a topical cream or gel, with cream being more commonly prescribed. It also can come as a vaginal cream or suppository. Estriol is formulated in our country (USA) at compounding pharmacies. Recently, one of our avid blog readers from Denmark told me that estriol is prescribed from their big box pharmacies. But currently, estriol is not found at the big box pharmacies in the USA. Most commonly estriol is combined with estradiol (biest) for hormone replacement. To learn more about estriol, see our blog: What is Estriol Used For?
Compounded formulation: Combinations of estrone, estradiol, and estriol.
-Triest is a formulation of the three bioidentical estrogens: estrone, estradiol, estriol. Triest is not used anymore. Estrone is not a healthy estrogen replacement and tends to have a lot of side effects. So Triest is not used anymore.
–Biest: Biest has since replaced triest for BHRT. Biest is a combination of estriol and estradiol. Biest is used because having estriol in the mix, reduces the potency of estradiol on the system. Estradiol is an amazing hormone and is helpful for hot flashes, night sweats, bone density, heart protective, memory and more. But estradiol can be quite strong and causes side effects if not properly managed. Estradiol alone can cause weight gain, strong appetite, irritability, uterine bleeding, breast tenderness. By combining estriol with estradiol, that can help reign in the negative effects of estradiol while still promoting the positive.
Biest Ratios: Biest can come in any forms or ratios of estriol and estradiol. The most common formulation of biest is an 80:20 ratio. An 80:20 ratio is 80% estriol to 20% ratio. For example, a 2.5mg of biest is a combination of estriol 2 mg with 0.5mg of estradiol. In some cases, a patient might need a different ratio of biest. For example, a female that is being transitioned from a conventional preparation of HRT like Premarin will need a higher ratio of estradiol to estriol. Most conventional preparations such as Premarin or even estradiol patches, there is more estradiol needed for the transition to biest BHRT. Using a traditional 80:20 of biest in a woman that is transitioning from Premarin or an estradiol patch will have a lot of menopausal symptoms. Simply because the estradiol is too weak for that type of patient.
Usually, I use a 50:50 ratio when transitioning from synthetic or conventional HRT to BHRT biest. Then with time, step down to an 80:20 ratio formulation of biest. In a patient that is experiencing menopausal symptoms and has never been on HRT, an 80:20 ratio of biest work the best. As stronger ratios such as a 50:50 ratio might cause unwanted estrogen dominance symptoms. Some women are extremely sensitive to estrogen and need a 90:10 ratio of biest. These women are so sensitive to estrogen that they have unwanted spotting, breast swelling, and tenderness, weight gain, and moodiness. Using more estriol over estradiol can resolve menopausal symptoms reducing unwanted symptoms.
Progesterone: Progesterone comes in many forms and doses. It is used for many conditions such as menopause, PMS, and PCOS.
Menopause: Usually in menopause estrogen is given. As mentioned above, if a female is taking estrogen and has a uterus, then she must take progesterone. Progesterone keeps the lining of the uterus thin which reduces the risk for uterine cancer. In a menopausal female that has a uterus and is taking estrogen, she must take progesterone orally to prevent and minimize the risk for uterine cancer. In most cases, progesterone cream (in any dose) is not sufficient enough to protect the uterus. Yes, there are exceptions to the rule and progesterone cream can be very potent.
But progesterone cream doesn’t have the effect on protecting the uterine lining from thickening like an oral dose. I say this over and over because I’ve had several patients that have gotten uterine cancer taking estrogen from other doctors without the proper form of progesterone. There is an exception to progesterone as a capsule versus a cream in menopause. That is the rhythmic dosing protocols of estradiol and progesterone creams. Rhythmic dosing is great for menopause, and I will talk about in a separate blog.
Progesterone is commonly taken at night. That is because progesterone is great for sleep and relaxing. Taking it at night is helpful for sleep. I have has a few patients that have accidentally taken their progesterone in the morning. Those are the times I get a phone call that they feel, “weird like they had a glass of wine.” Occasionally, I have some patients take progesterone in the morning. Those are the cases for the patient that have anxiety, or their uterus needs more protection from the estrogen they are taking.
For women that are not menopausal progesterone can be dosed in many forms. Progesterone is great for estrogen dominance to balance the estrogen and progesterone. Progesterone is also great for PMS and taken the last half of the cycle.
Like I mentioned, progesterone comes in many forms and dosings. Micronized progesterone can come from a compounding pharmacy in any dose the patient requires. I have used as little as 5 mg of progesterone up to 300 mg depending on the patient.
Sustained release progesterone: this is great to help a patient stay asleep through the night and seems to have more protection for the uterus. Instant release progesterone: this is great for someone that has trouble falling asleep. The instant release works so quickly that it help you fall asleep fast, but it doesn’t necessarily help you stay asleep.
Prometrium is the common form of progesterone from your gynecologist or primary care doc. Prometrium is an oral form and comes in the doses of 100mg and 200mg and is instant release. Because it is made from peanut oil, be careful about allergies. Sometime 100mg is too high for a patient or the instant release to strong. That is where a compounded formulation can be helpful.
How to Dose BHRT?
Many doctors will dose BHRT from both symptoms and lab work. The testing for hormones levels varies greatly as doctors have many different ways of testing. Many are staunchly opinionated about which hormone testing is best. I don’t think there is a perfect way of testing for hormones. I prefer blood testing. I have done blood testing since 2004 and have specific reference ranges that I look for. I like blood testing because most insurance companies will cover it. Out of pocket pricing through a physician’s lab account for hormone blood work is reasonable.
Other docs like to use saliva testing, urine testing, and blood spot testing. I am sure these are accurate methods of testing hormones. But I have used blood testing with my patients and feel very confident in prescribing based on those objective values and their subjective symptoms. In this post, I am going to explain how I dose hormones on blood testing values. Now take into consideration the patient’s subjective symptoms. But here is a quick synopsis of what I do, based on lab values from blood work.
Lab Testing: When I have patients do their blood test, they need to take their hormones 3-5 hours before the blood draw. This gives me an idea of how they are absorbing the BHRT. Many patients do not understand this and want to have their blood draw without taking their hormones that morning. But this tells me what their levels of hormones on their own. I want to see how they are absorbing the hormones I am prescribing them.
Menopause:
Estradiol: This depends on the patient. Most menopausal females do well with estradiol levels at 40-60. Testing the total-estrogens is not an accurate way of testing. It is important to make sure to test the estradiol. Some women do better on estradiol close to 90-100 which is why it is important to get their subjective symptoms.
Progesterone: Because most women take the progesterone at night and then have their blood draw in the morning, it is normal for the levels to look “low.” But a good 16 hours after taking the progesterone the levels should be 3-5. If a woman over menopausal age is spotting or having uterine bleeding, that means the progesterone is too low, or the estrogen is too high. You do not want a woman to have spotting or a period when on BHRT. There is an exception to this, in the case of rhythmic dosing. In a rhythmic BHRT dosing schedule, a woman is supposed to have a monthly period. Again, this is an entirely separate blog post. So if a patient is having spotting and not on rhythmic dosing, then raise the progesterone or lower the estrogen dose.
Testosterone:
WOMEN: Testosterone levels for women’s lab work are ridiculous. The common reference range is 2-45, which means a level of 2 is normal or a level of 45 is normal. This is a huge testosterone range for women. Most women feel very good at a testosterone level of 30-35. Testosterone is great for developing muscle mass, drive, ambition, and motivation. It is also really great for skin integrity. From my experience, testosterone can help sex drive, but it is not the be all end all for libido. I have had women taking testosterone with high levels, but their libido was nonexistent. While I find that estrogen is more effective for sex drive, testosterone can help. Ultimately the goal is to make sure the estrogen, progesterone, and testosterone levels are balanced. The deciding factor for dosing testosterone would be a woman’s symptoms. As every female is different on how they respond to testosterone. If a woman is having acne or breakout issues, then the testosterone is too high. If they start having hair loss, especially the temples and top of the head, the testosterone dose is too high. If a woman starts feeling “testy” or irritable not warranted for the situation, then the testosterone is too high. Testosterone should not be dosed orally as that is hard on the liver and not easily absorbed. Usually, it is best dosed as a transdermal cream. The interesting thing about testosterone is where you apply the cream, it can grow hair. It only stimulates the hair follicles where you apply it. I usually have patients apply their testosterone cream to the inner thigh or back of the knee. These locations prevent “sharing” the hormones with others and prevent unwanted hair growth. I have seen plenty of patients come in to see me with hairy arms. When I ask them if they apply their testosterone to their arms, they are surprised. But their hairy arms gave it away.
MEN: There are several formulation doses for men with low testosterone. Transdermal creams and gels are common as well as pellets and injections. I like to use rhythmic dosing of testosterone for men. It is a transdermal application of cream that is applied in different doses throughout the month. This rhythmic dosing will follow what a young male’s testosterone levels normally are. Yes, men actually cycle their testosterone like women do their estrogen and progesterone. Injection and pellets are used for Low T as well. But unfortunately, the body can be a bit lazy. Once you use a potent high dose form of testosterone like a pellet or injectable, it can turn off one’s own production. It is nearly impossible to get the male’s body to produce any testosterone on its own after pellets and injections.
Back to What is BHRT is used for?
I would like to delve into how BHRT can help the most common conditions for hormone replacement. Those conditions being the ones I referred to above, menopause, perimenopause, PMS, PCOS, Low Testosterone also abbreviated ‘LowT.’ The best way to explain this is to use examples of actual patients. These are common scenarios that a BHRT doctor might see, or you might resonate with yourself.
Patient Example 1 – Natural Menopause: Kelly is 51 years old and has not had her period in 4 months. She feels terrible because she cannot sleep due to the continuous, frequent night sweats. She has at least six hot flashes during the day. Kelly does not feel like herself. Her memory recall has disappeared, and she’s gained 15 lbs. She has been experiencing vaginal dryness, not to mention her sex drive is low anyway. Kelly’s personal and family history makes her a good candidate for BHRT. Because Kelly has never been on any hormone therapy before we were able to do a low dose of BHRT. She responded really well to a biest (80:20 ratio) of 2.5mg cream.
She did half in the morning and a half at night. Meaning Kelly applied a dose of 1.25mg of biest to her inner thigh in the morning and 1.25mg at night. This came to a total of 2.5mg of biest a day. That broken up into the 80:20 ratio equaled 2.0 mg of estriol and .5mg of estradiol total a day. Because Kelly had her uterus meant she needed an oral form of progesterone. Kelly would take a sustained release micronized 100mg or progesterone capsule at night. This protected and kept her uterine lining thin. This dose and formulation also helped her sleep through the entire night.
The BHRT dosing of biest (estriol and estradiol) also improved her symptoms of hot flashes and night sweats. It also helped her alleviate her brain fog. This dose helped improved her sex drive, but it did not help with her vaginal dryness. That is because taking a low dose BHRT cream, may not be enough for the vaginal tissues. It was not nice to improve Kelly’s sex drive but not help the vaginal pain and dryness with intercourse. In this case, I gave Kelly a separate estriol only vaginal cream 2mg per gram. She applied a half of a gram 1 mg twice a week to her vaginal tissues (at night). After six weeks this improved her vaginal dryness, and she no longer had pain with intercourse.
Patient Example 2 – Surgical Menopause: Melissa is 47 years old and just had a total hysterectomy/oophorectomy (removal of the uterus and both ovaries). She was having incredibly heavy periods due to multiple large fibroids. Melissa was bleeding so heavy for so long she was chronically anemic. Not to mention her quality of life was in the can because she was so tired, and worried that she might start to bleed or get her period at any moment (forget vacations or long road trips). Melissa’s gynecologist referred her to me after she could not tolerate the conventional medications he prescribed her. Not mention he didn’t feel comfortable prescribing estrogen to her.
After the total hysterectomy, Melissa was happy to not bleed constantly anymore. But Melissa felt terrible because she was experiencing “surgical menopause.” Surgical menopause is where the body goes from having a good amount of estrogen to absolutely nothing. This can cause severe menopausal symptoms. Kelly’s dose of BHRT would not have touched Melissa’s symptoms. I ended up giving Melissa an 80:20 ratio of biest at 8 mg per gram cream. She applied a 1/4 of a gram morning and ¾ gram in the evening. This equaled 2 mg morning and 6mg at night. I did this because Melissa needed more estrogen at night keep the night sweats at bay.
When we are sleeping, our immune system will raise up our body temperature to fight any viruses or pathogens we came into contact during the day. In a woman with hormonal imbalance, this rise in temperature will cause intense night sweats. I needed to give Melissa a little more estrogen at night to account for the night sweats. Many doctors believe if you do not have a uterus, you do not need progesterone. I completely disagree with this philosophy. Yes, I understand to protect the uterus from the risk of cancer, progesterone is necessary. Just because you do not have a uterus does not mean you don’t need progesterone.
Progesterone can help you stay asleep all through the night. It is also very good for mood, especially irritability. It also helps balance estrogen to prevent estrogen dominance. Estrogen dominance symptoms are weight gain, moodiness, sugar cravings, anxiety to mention a few. While the dose is determined by the patient’s symptoms, Melissa did well on 75 mg of oral progesterone. This dose for Melissa helped her sleep, mood and balanced the estrogen, so she lost weight and reduced her cravings.
Patient Example 3 – Conventional HRT transfer to BHRT: Mickey was on Premarin for 15 years. Mickey had a hysterectomy 15 years ago, and her doctor immediately put her on Premarin. She did really well on Premarin. She never had hot flashes, no vaginal dryness, great energy and felt pretty good. Her doctor retired, and her new doc would not under any circumstances prescribe her Premarin. In fact, Mickey’s new doctor would not prescribe any HRT. Understandably, after the WHI study in 2001, most doctors stopped prescribing Premarin and conventional HRT. But Mickey went from taking Premarin to taking nothing. She told me she wanted to jump off a bridge because her symptoms were so severe. This is not being dramatic. Going from synthetic/non-bioidentical hormones to nothing can be a drastic change. Imagine, intense hot flashes, no sleep, anxiety, hair loss, huge sugar cravings, irritability, and rage. That is just a few symptoms of going from non-bioidentical hormones to nothing. When you are transitioning a person from non-bioidentical hormones to BHRT, you have to go really strong. Otherwise, they will feel nothing. This is where BHRT gets a bad name. Most docs will not dose the BHRT high enough to get any real result.
This is what I did with Mickey:
-Estradiol only cream 8mg per gram. She did a half of a gram twice a day which equaled 4 mg morning and 4mg evening. She did well on this. It eliminated her hot flashes during the day. It helped her mood and irritability. She still had two really intense night sweats at night. But at least she got some sleep.
– After about 8-10 weeks I changed her dose to a biest 50:50 ratio. It was estriol 4mg with estradiol 4mg. This is called a biest 50:50 ratio of 8 mg per gram. She would apply a half of gram twice a day. This provides 2 mg estriol and 2 mg estradiol morning and evening. Mickey did well on this for the next six months. All hot flashes ceased, and she had no more night sweats. Her mood improved dramatically, and Mickey was really happy.
– After six months on the biest (50:50 ratio) 8mg, Mickey’s symptoms and blood work showed it was time to readjust her dose. Her estradiol was a little too high, and she started having some estrogen dominance symptoms. At this point I was able to reduce her dose to a biest (80:20 ratio) of 3 mg per gram, taking a half of a gram twice a day. 3mg per gram of biest (80:20) equals 2.4 mg estriol and 0.6 mg estradiol. Again, like Melissa, no uterus does not mean, no progesterone. I gave Mickey 50mg of progesterone, and it helped her sleep and mood.
Patient Example 4 – PMS: Premenstrual Syndrome can be detrimental for a woman and the people around them. See my blog: I am PMSing like crazy. It is usually the imbalance of estrogen to progesterone in the last half of the cycle. That is why women experience PMS anywhere from 3 to 14 days before their periods. Jackie is a perfect example of a patient I treated for PMS. She had PMS for 14 days before her period. Her symptoms were sugar cravings, irritability/rage, acne, weight gain, insomnia, and headaches. Jackie came in with her husband, Brian because her chief complaint was feeling really irritable. During days 14 to her period, Jackie would get cranky and blow up over the “littlest thing.” Jackie would easily get angry at Brian and their two children, Scarlett (8yo) and Michael (6yo). After blowing up “over nothing,” Jackie would feel guilty and then cry about the incident. Jackie’s primary care doctor had put her on antidepressants for her mood-issues, and she did terribly. Ultimately, she stopped the medication and ended up in my office looking for alternatives.
On day 21 of a perfect 28-day cycle, the progesterone level should be the highest of the entire month. To accurately test progesterone levels in a female, it should be done as close to day 21 of their cycle. On day 21 of Jackie’s cycle, the progesterone was nonexistent. Commonly, low progesterone can cause exacerbation of PMS symptoms. Because Jackie’s progesterone was so low, it gave her intense symptoms of PMS. One of the most common symptoms of low progesterone is irritability. To help Jackie, I gave her progesterone cream to take twice a day. Jackie took 50mg of progesterone cream twice a day from day 14 to her period. This helped her mood and sleep almost immediately. We also incorporated other lifestyle changes and adrenal support to help the sugar cravings, weight gain, and acne.
Patient Example 6 – Low Testosterone: Joe (56-year-old male) had been on testosterone injections for about two years since being diagnosed with Low T from his PCP. Joe recently stopped the testosterone injections because his girlfriend, Amanda felt like he was acting “aggro” and his sex drive was “too high.” And Joe did admit he wasn’t feeling quite right on the testosterone injections. On a quick side note: the testosterone molecule looks almost identical to the estradiol molecule. So it is common that testosterone can convert to estradiol. This conversion of estradiol is what usually causes the moodiness. Part of Joe’s symptoms might have been from the testosterone injections converting to estradiol. But when I saw Joe, he has been off the testosterone for two months.
At this time, he has no sex drive and was lethargic and had a low mood. He was more grumpy and just felt apathetic most of the time. Needless to say, Amanda wasn’t too thrilled with this side of Joe either. That is the hard part to testosterone injections and pellets. It is a high dose of testosterone that will inevitably turn off any and all production of testosterone. Sure a man might go on testosterone injections for low testosterone. But after taking testosterone injections, their testosterone levels will never be the same. Just like humans, the body is lazy. If you do the work, when you take it away the body will not bounce back. I tested Joe’s testosterone, and it was low.
In fact, to be honest, Joe’s testosterone was lower than the levels I keep women at for BHRT. For Joe, I gave him a static dose of testosterone cream with 10% DMSO. Men’s skin tends to be thicker than women’s so to help with absorption of hormones I have the compounding pharmacy add in DMSO. DMSO has been in use in the medical field for decades. By combining the testosterone with DMSO helps penetrate membranes/skin for better absorption. Testosterone cream for men doesn’t have the strong impact of injections and pellets. You can much more easily manipulate testosterone cream doses than injections or pellets. Bioidentical testosterone is a great way to provide hormones, but it doesn’t always have a long half-life. Which is why dosing the testosterone twice a day is important to keep the blood levels up. Joe ended up taking the testosterone cream with the DMSO twice a day. His energy and mood improved quite a bit. But he was not so irritable, which was great for him and Amanda’s relationship.
There is so much more to BHRT than what I have written here. In future posts, I will expand on this subject. I hope that this information has shed light on the many uses, formulations, and doses for hormone imbalances. If you have any comments for quesitons, please leave a comment below or send an email to [email protected]

































Hi, I’m 51 and I have been taking non bioidentical therapy for the pasted 8 years until May of 2019…. I had to stop taking do to bleeding… my gynecologist could not figure out why I was bleeding . My biopsy was negative, I had no polys or fibroids …and …I stop having periods at 48.. my gynecologist did a D&C on me and also an ablation…. after three weeks of recovery… than two clear weeks of nothing the bleeding started back….at that time I’m frustrated and aggravated… I immediately stop taking the hormonal pills…. than my hot flashes / night sweats / bad mood / dry eyes/ dry skin/ dry vagina began.. painful and burning sex /2 hour of sleep a night tired angry … you name it! Well three days ago my gynecologist recommended me to go to this .compounding pharmacy . Long story short …..im taking .5 estrogen in the AM and .6 progesterone at night… no changes yet … but after reading your article I’m wondering am I taking enough after come off the other therapy even tho 5 months had past….
Hello Tammy,
First off, bleeding while on hormones is totally normal. It happens a lot. It is either the estrogen dose is too high, or the progesterone dose is not high enough. The progesterone helps to inhibit the growth of the uterine lining so you don’t bleed. You mentioned in your message, ‘hormonal pills.” Is your estrogen still a pill? We do not prescribe Estradiol pills. Your dosing of 0.5 Estrogen and 0.6 of Progesterone both seem very low. We prefer to use Biest (estrogen) transdermal cream. In order to stop unpredictable bleeding, we usually use a bioidentical oral capsule of progesterone 100 mg. In your case, due to the bleeding, we would probably increase to 200 mg of bioidentical progesterone. Sorry you are having so much trouble.
Dr. Maki